Page 1118 - Basic _ Clinical Pharmacology ( PDFDrive )
P. 1118
1104 SECTION X Special Topics
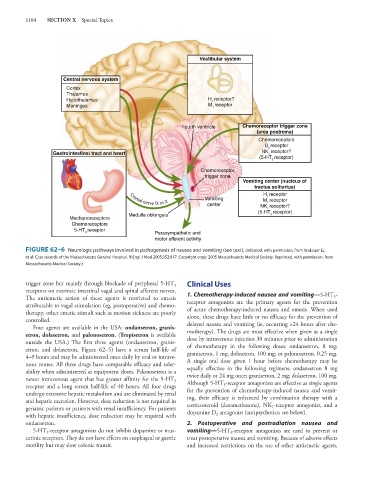
Vestibular system
Central nervous system
Cortex
Thalamus
Hypothalamus H receptor?
1
Meninges M receptor
1
Fourth ventricle Chemoreceptor trigger zone
(area postrema)
Chemoreceptors
D receptor
2
Gastrointestinal tract and heart NK receptor?
1
(5-HT receptor)
3
Chemoreceptor
trigger zone
Vomiting center (nucleus of
tractus solitarius)
H receptor
1
Vomiting M receptor
Cranial nerve IX or X
1
center NK receptor?
1
(5-HT receptor)
Medulla oblongata 3
Mechanoreceptors
Chemoreceptors
5-HT receptor Parasympathetic and
3
motor efferent activity
FIGURE 62–6 Neurologic pathways involved in pathogenesis of nausea and vomiting (see text). (Adapted, with permission, from Krakauer EL
et al: Case records of the Massachusetts General Hospital. N Engl J Med 2005;352:817. Copyright copy; 2005 Massachusetts Medical Society. Reprinted, with permission, from
Massachusetts Medical Society.)
trigger zone but mainly through blockade of peripheral 5-HT Clinical Uses
3
receptors on extrinsic intestinal vagal and spinal afferent nerves.
The antiemetic action of these agents is restricted to emesis 1. Chemotherapy-induced nausea and vomiting—5-HT -
3
attributable to vagal stimulation (eg, postoperative) and chemo- receptor antagonists are the primary agents for the prevention
therapy; other emetic stimuli such as motion sickness are poorly of acute chemotherapy-induced nausea and emesis. When used
controlled. alone, these drugs have little or no efficacy for the prevention of
Four agents are available in the USA: ondansetron, granis- delayed nausea and vomiting (ie, occurring >24 hours after che-
etron, dolasetron, and palonosetron. (Tropisetron is available motherapy). The drugs are most effective when given as a single
outside the USA.) The first three agents (ondansetron, granis- dose by intravenous injection 30 minutes prior to administration
etron, and dolasetron, Figure 62–5) have a serum half-life of of chemotherapy in the following doses: ondansetron, 8 mg;
4–9 hours and may be administered once daily by oral or intrave- granisetron, 1 mg; dolasetron, 100 mg; or palonosetron, 0.25 mg.
nous routes. All three drugs have comparable efficacy and toler- A single oral dose given 1 hour before chemotherapy may be
ability when administered at equipotent doses. Palonosetron is a equally effective in the following regimens: ondansetron 8 mg
newer intravenous agent that has greater affinity for the 5-HT twice daily or 24 mg once; granisetron, 2 mg; dolasetron, 100 mg.
3
receptor and a long serum half-life of 40 hours. All four drugs Although 5-HT -receptor antagonists are effective as single agents
3
undergo extensive hepatic metabolism and are eliminated by renal for the prevention of chemotherapy-induced nausea and vomit-
and hepatic excretion. However, dose reduction is not required in ing, their efficacy is enhanced by combination therapy with a
1
geriatric patients or patients with renal insufficiency. For patients corticosteroid (dexamethasone), NK -receptor antagonist, and a
2
with hepatic insufficiency, dose reduction may be required with dopamine D antagonist (antipsychotics; see below).
ondansetron. 2. Postoperative and postradiation nausea and
5-HT -receptor antagonists do not inhibit dopamine or mus- vomiting—5-HT -receptor antagonists are used to prevent or
3
3
carinic receptors. They do not have effects on esophageal or gastric treat postoperative nausea and vomiting. Because of adverse effects
motility but may slow colonic transit. and increased restrictions on the use of other antiemetic agents,