Page 363 - Basic _ Clinical Pharmacology ( PDFDrive )
P. 363
CHAPTER 20 Drugs Used in Asthma 349
Pathological
Activation stimulus intraluminal
(such as oxidant, Goblet cell mucus
virus or allergen) Eosinophil
Mucin
y e
ih
ye
p h
A Airway epithelium
Subepithelial mucosa TSLPR Goblet cell
metaplasia
TSLP, IL-25 and increased
DC and IL-33 epithelial
mucin stores Accumulation of
OX40L eosinophils, mast cells
expression and basophils
DC migration to
draining lymph node
ILC2
IL-5 and IL-13
production in the
airway epithelium and
Lymph subepithelial mucosa
node Mast cell
Basophil
OX40L B cell
OX40 follicle
IgE ‘arming’ of mast Pathological
cells and basophils changes in the airway
Naive T FH cell predispose to
CD4 + T cell B cell asthma exacerbation
Class-switching IgE
to IgE production T 2 cells
H
Plasma cell
Blood T H 2 cell
vessel
IgE B Cell
+
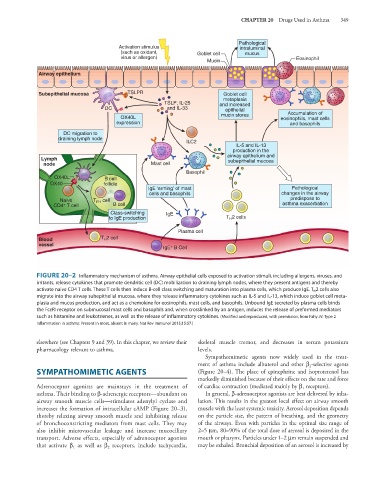
FIGURE 20–2 Inflammatory mechanism of asthma. Airway epithelial cells exposed to activation stimuli, including allergens, viruses, and
irritants, release cytokines that promote dendritic cell (DC) mobilization to draining lymph nodes, where they present antigens and thereby
activate naive CD4 T cells. These T cells then induce B-cell class switching and maturation into plasma cells, which produce IgE. T H 2 cells also
migrate into the airway subepithelial mucosa, where they release inflammatory cytokines such as IL-5 and IL-13, which induce goblet cell meta-
plasia and mucus production, and act as a chemokine for eosinophils, mast cells, and basophils. Unbound IgE secreted by plasma cells binds
the FcεRI receptor on submucosal mast cells and basophils and, when crosslinked by an antigen, induces the release of preformed mediators
such as histamine and leukotrienes, as well as the release of inflammatory cytokines. (Modified and reproduced, with permission, from Fahy JV: Type 2
inflammation in asthma: Present in most, absent in many. Nat Rev Immunol 2015;15:57.)
elsewhere (see Chapters 9 and 39). In this chapter, we review their skeletal muscle tremor, and decreases in serum potassium
pharmacology relevant to asthma. levels.
Sympathomimetic agents now widely used in the treat-
ment of asthma include albuterol and other β -selective agents
2
SYMPATHOMIMETIC AGENTS (Figure 20–4). The place of epinephrine and isoproterenol has
markedly diminished because of their effects on the rate and force
Adrenoceptor agonists are mainstays in the treatment of of cardiac contraction (mediated mainly by β receptors).
1
asthma. Their binding to β-adrenergic receptors—abundant on In general, β-adrenoceptor agonists are best delivered by inha-
airway smooth muscle cells—stimulates adenylyl cyclase and lation. This results in the greatest local effect on airway smooth
increases the formation of intracellular cAMP (Figure 20–3), muscle with the least systemic toxicity. Aerosol deposition depends
thereby relaxing airway smooth muscle and inhibiting release on the particle size, the pattern of breathing, and the geometry
of bronchoconstricting mediators from mast cells. They may of the airways. Even with particles in the optimal size range of
also inhibit microvascular leakage and increase mucociliary 2–5 μm, 80–90% of the total dose of aerosol is deposited in the
transport. Adverse effects, especially of adrenoceptor agonists mouth or pharynx. Particles under 1–2 μm remain suspended and
as well as β receptors, include tachycardia, may be exhaled. Bronchial deposition of an aerosol is increased by
that activate β 1 2