Page 477 - Basic _ Clinical Pharmacology ( PDFDrive )
P. 477
CHAPTER 26 Local Anesthetics 463
The amide local anesthetics undergo complex biotransforma-
Mepivacaine Intercostal tion in the liver, which includes hydroxylation and N-dealkylation
500 mg by liver microsomal cytochrome P450 isozymes. There is consid-
Caudal
Epidural erable variation in the rate of liver metabolism of individual amide
Brachial plexus compounds, with prilocaine (fastest) > lidocaine > mepivacaine >
ropivacaine ≈ bupivacaine and levobupivacaine (slowest). As a
Sciatic femoral
result, toxicity from amide-type local anesthetics is more likely
to occur in patients with hepatic disease. For example, the aver-
Lidocaine age elimination half-life of lidocaine may be increased from
400 mg Intercostal
Epidural 1.6 hours in normal patients (t , Table 26–2) to more than
½
6 hours in patients with severe liver disease. Many other drugs
Brachial plexus
used in anesthesia are metabolized by the same P450 isozymes,
Subcutaneous
and concomitant administration of these competing drugs may
slow the hepatic metabolism of the local anesthetics. Decreased
Prilocaine hepatic elimination of local anesthetics would also be anticipated
400 mg Intercostal in patients with reduced hepatic blood flow. For example, the
Caudal
hepatic elimination of lidocaine in patients anesthetized with
Epidural
volatile anesthetics (which reduce liver blood flow) is slower than
in patients anesthetized with intravenous anesthetic techniques.
Etidocaine Intercostal Delayed metabolism due to impaired hepatic blood flow may
300 mg
Caudal likewise occur in patients with heart failure.
Epidural
Brachial plexus Pharmacodynamics
A. Mechanism of Action
2 4 6 8 1. Membrane potential—The primary mechanism of action
Blood levels (mcg/mL)
of local anesthetics is blockade of voltage-gated sodium channels
(Figure 26–1). The excitable membrane of nerve axons, like the
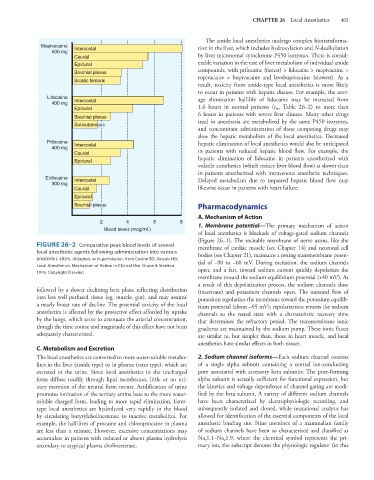
FIGURE 26–2 Comparative peak blood levels of several membrane of cardiac muscle (see Chapter 14) and neuronal cell
local anesthetic agents following administration into various bodies (see Chapter 21), maintains a resting transmembrane poten-
anatomic sites. (Adapted, with permission, from Covino BD, Vassals HG: tial of –90 to –60 mV. During excitation, the sodium channels
Local Anesthetics: Mechanism of Action in Clinical Use. Grune & Stratton,
1976. Copyright Elsevier.) open, and a fast, inward sodium current quickly depolarizes the
membrane toward the sodium equilibrium potential (+40 mV). As
a result of this depolarization process, the sodium channels close
followed by a slower declining beta phase reflecting distribution (inactivate) and potassium channels open. The outward flow of
into less well perfused tissue (eg, muscle, gut), and may assume potassium repolarizes the membrane toward the potassium equilib-
a nearly linear rate of decline. The potential toxicity of the local rium potential (about –95 mV); repolarization returns the sodium
anesthetics is affected by the protective effect afforded by uptake channels to the rested state with a characteristic recovery time
by the lungs, which serve to attenuate the arterial concentration, that determines the refractory period. The transmembrane ionic
though the time course and magnitude of this effect have not been gradients are maintained by the sodium pump. These ionic fluxes
adequately characterized. are similar to, but simpler than, those in heart muscle, and local
anesthetics have similar effects in both tissues.
C. Metabolism and Excretion
The local anesthetics are converted to more water-soluble metabo- 2. Sodium channel isoforms—Each sodium channel consists
lites in the liver (amide type) or in plasma (ester type), which are of a single alpha subunit containing a central ion-conducting
excreted in the urine. Since local anesthetics in the uncharged pore associated with accessory beta subunits. The pore-forming
form diffuse readily through lipid membranes, little or no uri- alpha subunit is actually sufficient for functional expression, but
nary excretion of the neutral form occurs. Acidification of urine the kinetics and voltage dependence of channel gating are modi-
promotes ionization of the tertiary amine base to the more water- fied by the beta subunit. A variety of different sodium channels
soluble charged form, leading to more rapid elimination. Ester- have been characterized by electrophysiologic recording, and
type local anesthetics are hydrolyzed very rapidly in the blood subsequently isolated and cloned, while mutational analysis has
by circulating butyrylcholinesterase to inactive metabolites. For allowed for identification of the essential components of the local
example, the half-lives of procaine and chloroprocaine in plasma anesthetic binding site. Nine members of a mammalian family
are less than a minute. However, excessive concentrations may of sodium channels have been so characterized and classified as
accumulate in patients with reduced or absent plasma hydrolysis Na 1.1–Na 1.9, where the chemical symbol represents the pri-
v
v
secondary to atypical plasma cholinesterase. mary ion, the subscript denotes the physiologic regulator (in this