Page 503 - Basic _ Clinical Pharmacology ( PDFDrive )
P. 503
CHAPTER 27 Skeletal Muscle Relaxants 489
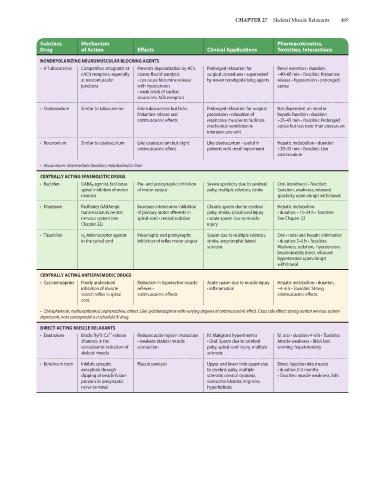
Subclass, Mechanism Pharmacokinetics,
Drug of Action Effects Clinical Applications Toxicities, Interactions
NONDEPOLARIZING NEUROMUSCULAR BLOCKING AGENTS
• d-Tubocurarine Competitive antagonist at Prevents depolarization by ACh, Prolonged relaxation for Renal excretion • duration,
nACh receptors, especially causes flaccid paralysis surgical procedures • superseded ~40–60 min • Toxicities: Histamine
at neuromuscular • can cause histamine release by newer nondepolarizing agents release • hypotension • prolonged
junctions with hypotension apnea
• weak block of cardiac
muscarinic ACh receptors
• Cisatracurium Similar to tubocurarine Like tubocurarine but lacks Prolonged relaxation for surgical Not dependent on renal or
histamine release and procedures • relaxation of hepatic function • duration
antimuscarinic effects respiratory muscles to facilitate ~25–45 min • Toxicities: Prolonged
mechanical ventilation in apnea but less toxic than atracurium
intensive care unit
• Rocuronium Similar to cisatracurium Like cisatracurium but slight Like cisatracurium • useful in Hepatic metabolism • duration
antimuscarinic effect patients with renal impairment ~20–35 min • Toxicities: Like
cisatracurium
• Vecuronium: Intermediate duration; metabolized in liver
CENTRALLY ACTING SPASMOLYTIC DRUGS
• Baclofen GABA B agonist, facilitates Pre- and postsynaptic inhibition Severe spasticity due to cerebral Oral, intrathecal • Toxicities:
spinal inhibition of motor of motor output palsy, multiple sclerosis, stroke Sedation, weakness; rebound
neurons spasticity upon abrupt withdrawal
• Diazepam Facilitates GABAergic Increases interneuron inhibition Chronic spasm due to cerebral Hepatic metabolism
transmission in central of primary motor afferents in palsy, stroke, spinal cord injury • duration ~12–24 h • Toxicities:
nervous system (see spinal cord • central sedation • acute spasm due to muscle See Chapter 22
Chapter 22) injury
• Tizanidine α 2 -Adrenoceptor agonist Presynaptic and postsynaptic Spasm due to multiple sclerosis, Oral • renal and hepatic elimination
in the spinal cord inhibition of reflex motor output stroke, amyotrophic lateral • duration 3–6 h • Toxicities:
sclerosis Weakness, sedation, hypotension,
hepatotoxicity (rare), rebound
hypertension upon abrupt
withdrawal
CENTRALLY ACTING ANTISPASMODIC DRUGS
• Cyclobenzaprine Poorly understood Reduction in hyperactive muscle Acute spasm due to muscle injury Hepatic metabolism • duration,
inhibition of muscle reflexes • • inflammation ~4–6 h • Toxicities: Strong
stretch reflex in spinal antimuscarinic effects antimuscarinic effects
cord
• Chlorphenesin, methocarbamol, orphenadrine, others: Like cyclobenzaprine with varying degrees of antimuscarinic effect. Class side effect: strong central nervous system
depression; note carisoprodol is a schedule IV drug.
DIRECT-ACTING MUSCLE RELAXANTS
2+
• Dantrolene Blocks RyR1 Ca -release Reduces actin-myosin interaction IV: Malignant hyperthermia IV, oral • duration 4–6 h • Toxicities:
channels in the • weakens skeletal muscle • Oral: Spasm due to cerebral Muscle weakness • Black box
sarcoplasmic reticulum of contraction palsy, spinal cord injury, multiple warning: hepatotoxicity
skeletal muscle sclerosis
• Botulinum toxin Inhibits synaptic Flaccid paralysis Upper and lower limb spasm due Direct injection into muscle
exocytosis through to cerebral palsy, multiple • duration 2–3 months
clipping of vesicle fusion sclerosis; cervical dystonia, • Toxicities: muscle weakness, falls
proteins in presynaptic overactive bladder, migraine,
nerve terminal hyperhidrosis