Page 3 - 53-Peptic ulcer diseases (Loét dạ dày)
P. 3
CHAPTER 53 Peptic Ulcer Disease 807
None known None known Serious ulcer-related complications often leading to hospitaliza-
tion occur in 1% to 4% of NSAID users. NSAID users who 53
15
ZES, other ZES, other
also take aspirin are at an especially high risk for complications.
NSAID In a population-based study from Denmark, the odds ratio for
use NSAID GI bleeding in people taking low-dose aspirin alone was 2.6, and
use this ratio increased to 5.6 in patients who were also taking an
NSAID. In a national study of mortality associated with a hos-
16
pital admission for adverse GI events related to NSAID use in
Spain, the death rate attributed to NSAID/aspirin use was 15.3
Hp Hp per 100,000 population compared to 2.5 per 100,000 of the gen-
infection infection
eral population. 17
The gastric and duodenal mucosa have several defense
mechanisms protecting them from digestion by acid and pep-
Duodenal Gastric sin (see Chapter 51). NSAIDs cause mucosal damage through
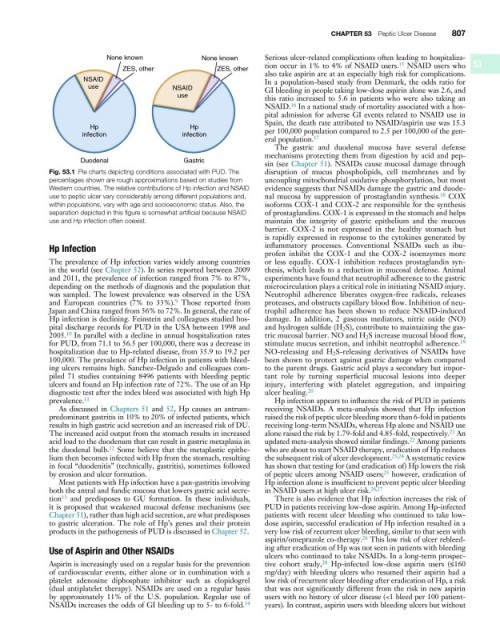
Fig. 53.1 Pie charts depicting conditions associated with PUD. The disruption of mucus phospholipids, cell membranes and by
percentages shown are rough approximations based on studies from uncoupling mitochondrial oxidative phosphorylation, but most
Western countries. The relative contributions of Hp infection and NSAID evidence suggests that NSAIDs damage the gastric and duode-
18
use to peptic ulcer vary considerably among different populations and, nal mucosa by suppression of prostaglandin synthesis. COX
within populations, vary with age and socioeconomic status. Also, the isoforms COX-1 and COX-2 are responsible for the synthesis
separation depicted in this figure is somewhat artificial because NSAID of prostaglandins. COX-1 is expressed in the stomach and helps
use and Hp infection often coexist. maintain the integrity of gastric epithelium and the mucous
barrier. COX-2 is not expressed in the healthy stomach but
is rapidly expressed in response to the cytokines generated by
Hp Infection inflammatory processes. Conventional NSAIDs such as ibu-
profen inhibit the COX-1 and the COX-2 isoenzymes more
The prevalence of Hp infection varies widely among countries or less equally. COX-1 inhibition reduces prostaglandin syn-
in the world (see Chapter 52). In series reported between 2009 thesis, which leads to a reduction in mucosal defense. Animal
and 2011, the prevalence of infection ranged from 7% to 87%, experiments have found that neutrophil adherence to the gastric
depending on the methods of diagnosis and the population that microcirculation plays a critical role in initiating NSAID injury.
was sampled. The lowest prevalence was observed in the USA Neutrophil adherence liberates oxygen-free radicals, releases
9
and European countries (7% to 33%). Those reported from proteases, and obstructs capillary blood flow. Inhibition of neu-
Japan and China ranged from 56% to 72%. In general, the rate of trophil adherence has been shown to reduce NSAID-induced
Hp infection is declining. Feinstein and colleagues studied hos- damage. In addition, 2 gaseous mediators, nitric oxide (NO)
pital discharge records for PUD in the USA between 1998 and and hydrogen sulfide (H 2 S), contribute to maintaining the gas-
10
2005. In parallel with a decline in annual hospitalization rates tric mucosal barrier. NO and H 2 S increase mucosal blood flow,
19
for PUD, from 71.1 to 56.5 per 100,000, there was a decrease in stimulate mucus secretion, and inhibit neutrophil adherence.
hospitalization due to Hp-related disease, from 35.9 to 19.2 per NO-releasing and H 2 S-releasing derivatives of NSAIDs have
100,000. The prevalence of Hp infection in patients with bleed- been shown to protect against gastric damage when compared
ing ulcers remains high. Sanchez-Delgado and colleagues com- to the parent drugs. Gastric acid plays a secondary but impor-
piled 71 studies containing 8496 patients with bleeding peptic tant role by turning superficial mucosal lesions into deeper
ulcers and found an Hp infection rate of 72%. The use of an Hp injury, interfering with platelet aggregation, and impairing
diagnostic test after the index bleed was associated with high Hp ulcer healing. 20
prevalence. 11 Hp infection appears to influence the risk of PUD in patients
As discussed in Chapters 51 and 52, Hp causes an antrum- receiving NSAIDs. A meta-analysis showed that Hp infection
predominant gastritis in 10% to 20% of infected patients, which raised the risk of peptic ulcer bleeding more than 6-fold in patients
results in high gastric acid secretion and an increased risk of DU. receiving long-term NSAIDs, whereas Hp alone and NSAID use
The increased acid output from the stomach results in increased alone raised the risk by 1.79-fold and 4.85-fold, respectively. An
21
22
acid load to the duodenum that can result in gastric metaplasia in updated meta-analysis showed similar findings. Among patients
the duodenal bulb. Some believe that the metaplastic epithe- who are about to start NSAID therapy, eradication of Hp reduces
12
lium then becomes infected with Hp from the stomach, resulting the subsequent risk of ulcer development. 23,24 A systematic review
in focal “duodenitis” (technically, gastritis), sometimes followed has shown that testing for (and eradication of) Hp lowers the risk
25
by erosion and ulcer formation. of peptic ulcers among NSAID users; however, eradication of
Most patients with Hp infection have a pan-gastritis involving Hp infection alone is insufficient to prevent peptic ulcer bleeding
both the antral and fundic mucosa that lowers gastric acid secre- in NSAID users at high ulcer risk. 26,27
tion and predisposes to GU formation. In these individuals, There is also evidence that Hp infection increases the risk of
13
it is proposed that weakened mucosal defense mechanisms (see PUD in patients receiving low-dose aspirin. Among Hp-infected
Chapter 51), rather than high acid secretion, are what predisposes patients with recent ulcer bleeding who continued to take low-
to gastric ulceration. The role of Hp’s genes and their protein dose aspirin, successful eradication of Hp infection resulted in a
products in the pathogenesis of PUD is discussed in Chapter 52. very low risk of recurrent ulcer bleeding, similar to that seen with
aspirin/omeprazole co-therapy. This low risk of ulcer rebleed-
26
Use of Aspirin and Other NSAIDs ing after eradication of Hp was not seen in patients with bleeding
ulcers who continued to take NSAIDs. In a long-term prospec-
28
Aspirin is increasingly used on a regular basis for the prevention tive cohort study, Hp-infected low-dose aspirin users (≤160
of cardiovascular events, either alone or in combination with a mg/day) with bleeding ulcers who resumed their aspirin had a
platelet adenosine diphosphate inhibitor such as clopidogrel low risk of recurrent ulcer bleeding after eradication of Hp, a risk
(dual antiplatelet therapy). NSAIDs are used on a regular basis that was not significantly different from the risk in new aspirin
by approximately 11% of the U.S. population. Regular use of users with no history of ulcer disease (<1 bleed per 100 patient-
14
NSAIDs increases the odds of GI bleeding up to 5- to 6-fold. years). In contrast, aspirin users with bleeding ulcers but without