Page 4 - 53-Peptic ulcer diseases (Loét dạ dày)
P. 4
808 PART VI Stomach and Duodenum
A B
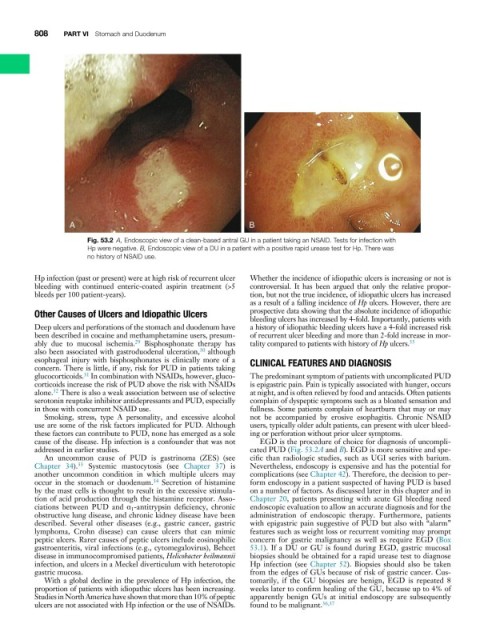
Fig. 53.2 A, Endoscopic view of a clean-based antral GU in a patient taking an NSAID. Tests for infection with
Hp were negative. B, Endoscopic view of a DU in a patient with a positive rapid urease test for Hp. There was
no history of NSAID use.
Hp infection (past or present) were at high risk of recurrent ulcer Whether the incidence of idiopathic ulcers is increasing or not is
bleeding with continued enteric-coated aspirin treatment (>5 controversial. It has been argued that only the relative propor-
bleeds per 100 patient-years). tion, but not the true incidence, of idiopathic ulcers has increased
as a result of a falling incidence of Hp ulcers. However, there are
Other Causes of Ulcers and Idiopathic Ulcers prospective data showing that the absolute incidence of idiopathic
bleeding ulcers has increased by 4-fold. Importantly, patients with
Deep ulcers and perforations of the stomach and duodenum have a history of idiopathic bleeding ulcers have a 4-fold increased risk
been described in cocaine and methamphetamine users, presum- of recurrent ulcer bleeding and more than 2-fold increase in mor-
35
29
ably due to mucosal ischemia. Bisphosphonate therapy has tality compared to patients with history of Hp ulcers.
also been associated with gastroduodenal ulceration, although
30
esophageal injury with bisphosphonates is clinically more of a CLINICAL FEATURES AND DIAGNOSIS
concern. There is little, if any, risk for PUD in patients taking
31
glucocorticoids. In combination with NSAIDs, however, gluco- The predominant symptom of patients with uncomplicated PUD
corticoids increase the risk of PUD above the risk with NSAIDs is epigastric pain. Pain is typically associated with hunger, occurs
alone. There is also a weak association between use of selective at night, and is often relieved by food and antacids. Often patients
32
serotonin reuptake inhibitor antidepressants and PUD, especially complain of dyspeptic symptoms such as a bloated sensation and
in those with concurrent NSAID use. fullness. Some patients complain of heartburn that may or may
Smoking, stress, type A personality, and excessive alcohol not be accompanied by erosive esophagitis. Chronic NSAID
use are some of the risk factors implicated for PUD. Although users, typically older adult patients, can present with ulcer bleed-
these factors can contribute to PUD, none has emerged as a sole ing or perforation without prior ulcer symptoms.
cause of the disease. Hp infection is a confounder that was not EGD is the procedure of choice for diagnosis of uncompli-
addressed in earlier studies. cated PUD (Fig. 53.2A and B). EGD is more sensitive and spe-
An uncommon cause of PUD is gastrinoma (ZES) (see cific than radiologic studies, such as UGI series with barium.
33
Chapter 34). Systemic mastocytosis (see Chapter 37) is Nevertheless, endoscopy is expensive and has the potential for
another uncommon condition in which multiple ulcers may complications (see Chapter 42). Therefore, the decision to per-
34
occur in the stomach or duodenum. Secretion of histamine form endoscopy in a patient suspected of having PUD is based
by the mast cells is thought to result in the excessive stimula- on a number of factors. As discussed later in this chapter and in
tion of acid production through the histamine receptor. Asso- Chapter 20, patients presenting with acute GI bleeding need
ciations between PUD and α 1 -antitrypsin deficiency, chronic endoscopic evaluation to allow an accurate diagnosis and for the
obstructive lung disease, and chronic kidney disease have been administration of endoscopic therapy. Furthermore, patients
described. Several other diseases (e.g., gastric cancer, gastric with epigastric pain suggestive of PUD but also with “alarm”
lymphoma, Crohn disease) can cause ulcers that can mimic features such as weight loss or recurrent vomiting may prompt
peptic ulcers. Rarer causes of peptic ulcers include eosinophilic concern for gastric malignancy as well as require EGD (Box
gastroenteritis, viral infections (e.g., cytomegalovirus), Behcet 53.1). If a DU or GU is found during EGD, gastric mucosal
disease in immunocompromised patients, Helicobacter heilmannii biopsies should be obtained for a rapid urease test to diagnose
infection, and ulcers in a Meckel diverticulum with heterotopic Hp infection (see Chapter 52). Biopsies should also be taken
gastric mucosa. from the edges of GUs because of risk of gastric cancer. Cus-
With a global decline in the prevalence of Hp infection, the tomarily, if the GU biopsies are benign, EGD is repeated 8
proportion of patients with idiopathic ulcers has been increasing. weeks later to confirm healing of the GU, because up to 4% of
Studies in North America have shown that more than 10% of peptic apparently benign GUs at initial endoscopy are subsequently
ulcers are not associated with Hp infection or the use of NSAIDs. found to be malignant. 36,37