Page 24 - Acute Pancreatitis (Viêm tụy cấp)
P. 24
CHAPTER 58 Acute Pancreatitis 915
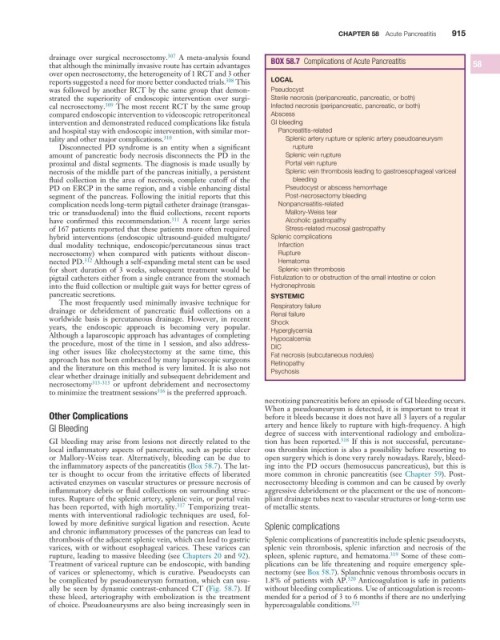
drainage over surgical necrosectomy. 307 A meta-analysis found BOX 58 .7 Complications of Acute Pancreatitis
that although the minimally invasive route has certain advantages 58
over open necrosectomy, the heterogeneity of 1 RCT and 3 other
reports suggested a need for more better conducted trials. 308 This LOCAL
was followed by another RCT by the same group that demon- Pseudocyst
strated the superiority of endoscopic intervention over surgi- Sterile necrosis (peripancreatic, pancreatic, or both)
cal necrosectomy. 309 The most recent RCT by the same group Infected necrosis (peripancreatic, pancreatic, or both)
compared endoscopic intervention to videoscopic retroperitoneal Abscess
intervention and demonstrated reduced complications like fistula GI bleeding
and hospital stay with endoscopic intervention, with similar mor- Pancreatitis-related
tality and other major complications. 310 Splenic artery rupture or splenic artery pseudoaneurysm
Disconnected PD syndrome is an entity when a significant rupture
amount of pancreatic body necrosis disconnects the PD in the Splenic vein rupture
proximal and distal segments. The diagnosis is made usually by Portal vein rupture
necrosis of the middle part of the pancreas initially, a persistent Splenic vein thrombosis leading to gastroesophageal variceal
fluid collection in the area of necrosis, complete cutoff of the bleeding
PD on ERCP in the same region, and a viable enhancing distal Pseudocyst or abscess hemorrhage
segment of the pancreas. Following the initial reports that this Post-necrosectomy bleeding
complication needs long-term pigtail catheter drainage (transgas- Nonpancreatitis-related
tric or transduodenal) into the fluid collections, recent reports Mallory-Weiss tear
have confirmed this recommendation. 311 A recent large series Alcoholic gastropathy
of 167 patients reported that these patients more often required Stress-related mucosal gastropathy
hybrid interventions (endoscopic ultrasound-guided multigate/ Splenic complications
dual modality technique, endoscopic/percutaneous sinus tract Infarction
necrosectomy) when compared with patients without discon- Rupture
nected PD. 312 Although a self-expanding metal stent can be used Hematoma
for short duration of 3 weeks, subsequent treatment would be Splenic vein thrombosis
pigtail catheters either from a single entrance from the stomach Fistulization to or obstruction of the small intestine or colon
into the fluid collection or multiple gait ways for better egress of Hydronephrosis
pancreatic secretions. SYSTEMIC
The most frequently used minimally invasive technique for
drainage or debridement of pancreatic fluid collections on a Respiratory failure
Renal failure
worldwide basis is percutaneous drainage. However, in recent Shock
years, the endoscopic approach is becoming very popular. Hyperglycemia
Although a laparoscopic approach has advantages of completing Hypocalcemia
the procedure, most of the time in 1 session, and also address- DIC
ing other issues like cholecystectomy at the same time, this Fat necrosis (subcutaneous nodules)
approach has not been embraced by many laparoscopic surgeons Retinopathy
and the literature on this method is very limited. It is also not Psychosis
clear whether drainage initially and subsequent debridement and
necrosectomy 313-315 or upfront debridement and necrosectomy
to minimize the treatment sessions 316 is the preferred approach.
necrotizing pancreatitis before an episode of GI bleeding occurs.
When a pseudoaneurysm is detected, it is important to treat it
Other Complications before it bleeds because it does not have all 3 layers of a regular
GI Bleeding artery and hence likely to rupture with high-frequency. A high
degree of success with interventional radiology and emboliza-
GI bleeding may arise from lesions not directly related to the tion has been reported. 318 If this is not successful, percutane-
local inflammatory aspects of pancreatitis, such as peptic ulcer ous thrombin injection is also a possibility before resorting to
or Mallory-Weiss tear. Alternatively, bleeding can be due to open surgery which is done very rarely nowadays. Rarely, bleed-
the inflammatory aspects of the pancreatitis (Box 58.7). The lat- ing into the PD occurs (hemosuccus pancreaticus), but this is
ter is thought to occur from the irritative effects of liberated more common in chronic pancreatitis (see Chapter 59). Post-
activated enzymes on vascular structures or pressure necrosis of necrosectomy bleeding is common and can be caused by overly
inflammatory debris or fluid collections on surrounding struc- aggressive debridement or the placement or the use of noncom-
tures. Rupture of the splenic artery, splenic vein, or portal vein pliant drainage tubes next to vascular structures or long-term use
has been reported, with high mortality. 317 Temporizing treat- of metallic stents.
ments with interventional radiologic techniques are used, fol-
lowed by more definitive surgical ligation and resection. Acute Splenic complications
and chronic inflammatory processes of the pancreas can lead to
thrombosis of the adjacent splenic vein, which can lead to gastric Splenic complications of pancreatitis include splenic pseudocysts,
varices, with or without esophageal varices. These varices can splenic vein thrombosis, splenic infarction and necrosis of the
rupture, leading to massive bleeding (see Chapters 20 and 92). spleen, splenic rupture, and hematoma. 319 Some of these com-
Treatment of variceal rupture can be endoscopic, with banding plications can be life threatening and require emergency sple-
of varices or splenectomy, which is curative. Pseudocysts can nectomy (see Box 58.7). Splanchnic venous thrombosis occurs in
be complicated by pseudoaneurysm formation, which can usu- 1.8% of patients with AP. 320 Anticoagulation is safe in patients
ally be seen by dynamic contrast-enhanced CT (Fig. 58.7). If without bleeding complications. Use of anticoagulation is recom-
these bleed, arteriography with embolization is the treatment mended for a period of 3 to 6 months if there are no underlying
of choice. Pseudoaneurysms are also being increasingly seen in hypercoagulable conditions. 321