Page 3 - Acute Pancreatitis (Viêm tụy cấp)
P. 3
894 PART VII Pancreas
BOX 58 .1 2012 Atlanta Classification Revision of Acute
Pancreatitis 12
MILD ACUTE PANCREATITIS
No organ failure
No local or systemic complications
MODERATELY SEVERE ACUTE PANCREATITIS
Transient organ failure (<48 hr) and/or G
Local or systemic complications* without persistent organ failure
SEVERE ACUTE PANCREATITIS P
Persistent organ failure (>48 hr) ___ single organ or multiorgan
*Local complications are peripancreatic fluid collections, pancreatic necrosis
and peripancreatic necrosis (sterile or infected), pseudocyst, and walled-
off necrosis (sterile or infected).
DEFINITIONS
10
The 1992 Atlanta Symposium served physicians involved in car-
ing for patients with AP well for nearly 2 decades, but subsequent
advancements about various aspects of the disease necessitated the
11
recent consensus revision. Whereas AP is best defined physiologi-
cally as an acute inflammatory process of the pancreas with variable
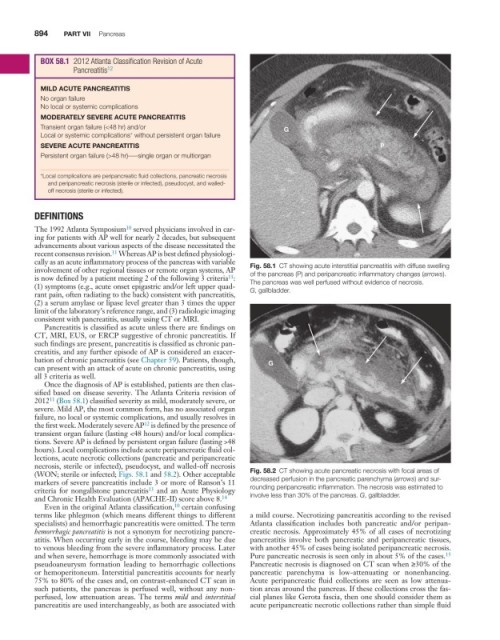
involvement of other regional tissues or remote organ systems, AP Fig. 58.1 CT showing acute interstitial pancreatitis with diffuse swelling
11
is now defined by a patient meeting 2 of the following 3 criteria : of the pancreas (P) and peripancreatic inflammatory changes (arrows).
(1) symptoms (e.g., acute onset epigastric and/or left upper quad- The pancreas was well perfused without evidence of necrosis.
rant pain, often radiating to the back) consistent with pancreatitis, G, gallbladder.
(2) a serum amylase or lipase level greater than 3 times the upper
limit of the laboratory’s reference range, and (3) radiologic imaging
consistent with pancreatitis, usually using CT or MRI.
Pancreatitis is classified as acute unless there are findings on
CT, MRI, EUS, or ERCP suggestive of chronic pancreatitis. If
such findings are present, pancreatitis is classified as chronic pan-
creatitis, and any further episode of AP is considered an exacer-
bation of chronic pancreatitis (see Chapter 59). Patients, though, G
can present with an attack of acute on chronic pancreatitis, using
all 3 criteria as well.
Once the diagnosis of AP is established, patients are then clas-
sified based on disease severity. The Atlanta Criteria revision of
11
2012 (Box 58.1) classified severity as mild, moderately severe, or
severe. Mild AP, the most common form, has no associated organ
failure, no local or systemic complications, and usually resolves in
the first week. Moderately severe AP is defined by the presence of
12
transient organ failure (lasting <48 hours) and/or local complica-
tions. Severe AP is defined by persistent organ failure (lasting >48
hours). Local complications include acute peripancreatic fluid col-
lections, acute necrotic collections (pancreatic and peripancreatic
necrosis, sterile or infected), pseudocyst, and walled-off necrosis
(WON; sterile or infected; Figs. 58.1 and 58.2). Other acceptable Fig. 58.2 CT showing acute pancreatic necrosis with focal areas of
markers of severe pancreatitis include 3 or more of Ranson’s 11 decreased perfusion in the pancreatic parenchyma (arrows) and sur-
criteria for nongallstone pancreatitis and an Acute Physiology rounding peripancreatic inflammation. The necrosis was estimated to
13
and Chronic Health Evaluation (APACHE-II) score above 8. 14 involve less than 30% of the pancreas. G, gallbladder.
10
Even in the original Atlanta classification, certain confusing
terms like phlegmon (which means different things to different a mild course. Necrotizing pancreatitis according to the revised
specialists) and hemorrhagic pancreatitis were omitted. The term Atlanta classification includes both pancreatic and/or peripan-
hemorrhagic pancreatitis is not a synonym for necrotizing pancre- creatic necrosis. Approximately 45% of all cases of necrotizing
atitis. When occurring early in the course, bleeding may be due pancreatitis involve both pancreatic and peripancreatic tissues,
to venous bleeding from the severe inflammatory process. Later with another 45% of cases being isolated peripancreatic necrosis.
and when severe, hemorrhage is more commonly associated with Pure pancreatic necrosis is seen only in about 5% of the cases.
15
pseudoaneurysm formation leading to hemorrhagic collections Pancreatic necrosis is diagnosed on CT scan when ≥30% of the
or hemoperitoneum. Interstitial pancreatitis accounts for nearly pancreatic parenchyma is low-attenuating or nonenhancing.
75% to 80% of the cases and, on contrast-enhanced CT scan in Acute peripancreatic fluid collections are seen as low attenua-
such patients, the pancreas is perfused well, without any non- tion areas around the pancreas. If these collections cross the fas-
perfused, low attenuation areas. The terms mild and interstitial cial planes like Gerota fascia, then one should consider them as
pancreatitis are used interchangeably, as both are associated with acute peripancreatic necrotic collections rather than simple fluid