Page 7 - Acute Pancreatitis (Viêm tụy cấp)
P. 7
898 PART VII Pancreas
62
a biliary cause. AP is rare in pregnancy, occurring most com-
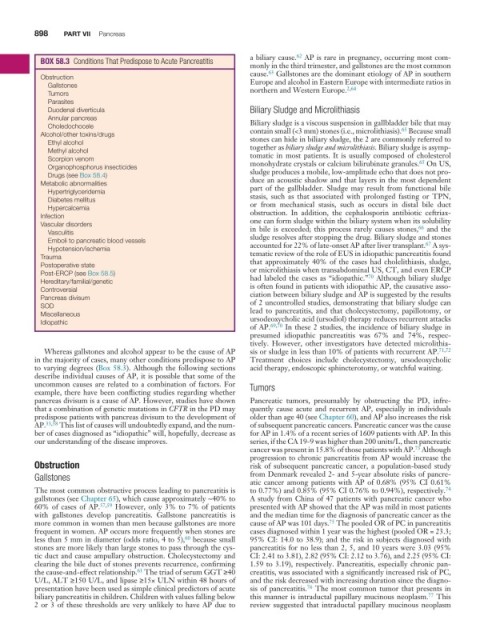
BOX 58 .3 Conditions That Predispose to Acute Pancreatitis
monly in the third trimester, and gallstones are the most common
63
cause. Gallstones are the dominant etiology of AP in southern
Obstruction Europe and alcohol in Eastern Europe with intermediate ratios in
Gallstones northern and Western Europe. 2,64
Tumors
Parasites
Duodenal diverticula Biliary Sludge and Microlithiasis
Annular pancreas Biliary sludge is a viscous suspension in gallbladder bile that may
Choledochocele 65
Alcohol/other toxins/drugs contain small (<3 mm) stones (i.e., microlithiasis). Because small
stones can hide in biliary sludge, the 2 are commonly referred to
Ethyl alcohol together as biliary sludge and microlithiasis. Biliary sludge is asymp-
Methyl alcohol tomatic in most patients. It is usually composed of cholesterol
Scorpion venom monohydrate crystals or calcium bilirubinate granules. On US,
65
Organophosphorus insecticides sludge produces a mobile, low-amplitude echo that does not pro-
Drugs (see Box 58.4)
Metabolic abnormalities duce an acoustic shadow and that layers in the most dependent
part of the gallbladder. Sludge may result from functional bile
Hypertriglyceridemia stasis, such as that associated with prolonged fasting or TPN,
Diabetes mellitus or from mechanical stasis, such as occurs in distal bile duct
Hypercalcemia
Infection obstruction. In addition, the cephalosporin antibiotic ceftriax-
one can form sludge within the biliary system when its solubility
Vascular disorders in bile is exceeded; this process rarely causes stones, and the
66
Vasculitis sludge resolves after stopping the drug. Biliary sludge and stones
Emboli to pancreatic blood vessels accounted for 22% of late-onset AP after liver transplant. A sys-
67
Hypotension/ischemia
Trauma tematic review of the role of EUS in idiopathic pancreatitis found
that approximately 40% of the cases had cholelithiasis, sludge,
Postoperative state or microlithiasis when transabdominal US, CT, and even ERCP
Post-ERCP (see Box 58.5) had labeled the cases as “idiopathic.” Although biliary sludge
70
Hereditary/familial/genetic is often found in patients with idiopathic AP, the causative asso-
Controversial ciation between biliary sludge and AP is suggested by the results
Pancreas divisum of 2 uncontrolled studies, demonstrating that biliary sludge can
SOD lead to pancreatitis, and that cholecystectomy, papillotomy, or
Miscellaneous ursodeoxycholic acid (ursodiol) therapy reduces recurrent attacks
Idiopathic
of AP. 69,70 In these 2 studies, the incidence of biliary sludge in
presumed idiopathic pancreatitis was 67% and 74%, respec-
tively. However, other investigators have detected microlithia-
Whereas gallstones and alcohol appear to be the cause of AP sis or sludge in less than 10% of patients with recurrent AP. 71,72
in the majority of cases, many other conditions predispose to AP Treatment choices include cholecystectomy, ursodeoxycholic
to varying degrees (Box 58.3). Although the following sections acid therapy, endoscopic sphincterotomy, or watchful waiting.
describe individual causes of AP, it is possible that some of the
uncommon causes are related to a combination of factors. For Tumors
example, there have been conflicting studies regarding whether
pancreas divisum is a cause of AP. However, studies have shown Pancreatic tumors, presumably by obstructing the PD, infre-
that a combination of genetic mutations in CFTR in the PD may quently cause acute and recurrent AP, especially in individuals
predispose patients with pancreas divisum to the development of older than age 40 (see Chapter 60), and AP also increases the risk
AP. 33,58 This list of causes will undoubtedly expand, and the num- of subsequent pancreatic cancers. Pancreatic cancer was the cause
ber of cases diagnosed as “idiopathic” will, hopefully, decrease as for AP in 1.4% of a recent series of 1609 patients with AP. In this
our understanding of the disease improves. series, if the CA 19-9 was higher than 200 units/L, then pancreatic
73
cancer was present in 15.8% of those patients with AP. Although
progression to chronic pancreatitis from AP would increase the
Obstruction risk of subsequent pancreatic cancer, a population-based study
Gallstones from Denmark revealed 2- and 5-year absolute risks of pancre-
atic cancer among patients with AP of 0.68% (95% CI 0.61%
74
The most common obstructive process leading to pancreatitis is to 0.77%) and 0.85% (95% CI 0.76% to 0.94%), respectively.
gallstones (see Chapter 65), which cause approximately ∼40% to A study from China of 47 patients with pancreatic cancer who
60% of cases of AP. 57,59 However, only 3% to 7% of patients presented with AP showed that the AP was mild in most patients
with gallstones develop pancreatitis. Gallstone pancreatitis is and the median time for the diagnosis of pancreatic cancer as the
75
more common in women than men because gallstones are more cause of AP was 101 days. The pooled OR of PC in pancreatitis
frequent in women. AP occurs more frequently when stones are cases diagnosed within 1 year was the highest (pooled OR = 23.3;
60
less than 5 mm in diameter (odds ratio, 4 to 5), because small 95% CI: 14.0 to 38.9); and the risk in subjects diagnosed with
stones are more likely than large stones to pass through the cys- pancreatitis for no less than 2, 5, and 10 years were 3.03 (95%
tic duct and cause ampullary obstruction. Cholecystectomy and CI: 2.41 to 3.81), 2.82 (95% CI: 2.12 to 3.76), and 2.25 (95% CI:
clearing the bile duct of stones prevents recurrence, confirming 1.59 to 3.19), respectively. Pancreatitis, especially chronic pan-
the cause-and-effect relationship. The triad of serum GGT ≥40 creatitis, was associated with a significantly increased risk of PC,
61
U/L, ALT ≥150 U/L, and lipase ≥15× ULN within 48 hours of and the risk decreased with increasing duration since the diagno-
76
presentation have been used as simple clinical predictors of acute sis of pancreatitis. The most common tumor that presents in
77
biliary pancreatitis in children. Children with values falling below this manner is intraductal papillary mucinous neoplasm. This
2 or 3 of these thresholds are very unlikely to have AP due to review suggested that intraductal papillary mucinous neoplasm