Page 9 - Acute Pancreatitis (Viêm tụy cấp)
P. 9
900 PART VII Pancreas
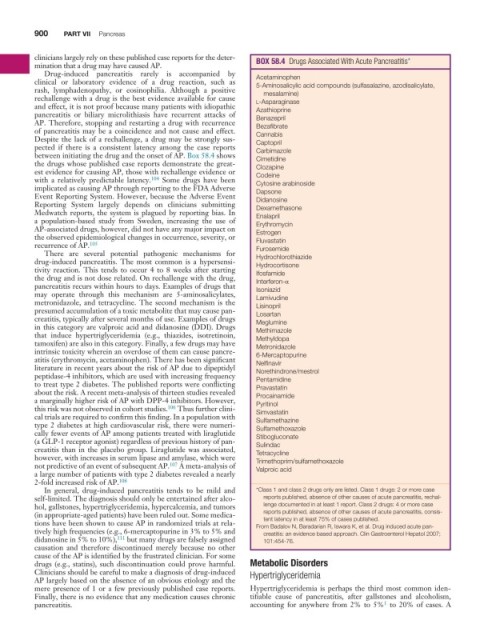
clinicians largely rely on these published case reports for the deter- BOX 58 .4 Drugs Associated With Acute Pancreatitis*
mination that a drug may have caused AP.
Drug-induced pancreatitis rarely is accompanied by
clinical or laboratory evidence of a drug reaction, such as Acetaminophen
5-Aminosalicylic acid compounds (sulfasalazine, azodisalicylate,
rash, lymphadenopathy, or eosinophilia. Although a positive mesalamine)
rechallenge with a drug is the best evidence available for cause l-Asparaginase
and effect, it is not proof because many patients with idiopathic Azathioprine
pancreatitis or biliary microlithiasis have recurrent attacks of Benazepril
AP. Therefore, stopping and restarting a drug with recurrence Bezafibrate
of pancreatitis may be a coincidence and not cause and effect. Cannabis
Despite the lack of a rechallenge, a drug may be strongly sus- Captopril
pected if there is a consistent latency among the case reports Carbimazole
between initiating the drug and the onset of AP. Box 58.4 shows Cimetidine
the drugs whose published case reports demonstrate the great- Clozapine
est evidence for causing AP, those with rechallenge evidence or Codeine
with a relatively predictable latency. 104 Some drugs have been Cytosine arabinoside
implicated as causing AP through reporting to the FDA Adverse Dapsone
Event Reporting System. However, because the Adverse Event Didanosine
Reporting System largely depends on clinicians submitting Dexamethasone
Medwatch reports, the system is plagued by reporting bias. In Enalapril
a population-based study from Sweden, increasing the use of Erythromycin
AP-associated drugs, however, did not have any major impact on Estrogen
the observed epidemiological changes in occurrence, severity, or Fluvastatin
recurrence of AP. 105 Furosemide
There are several potential pathogenic mechanisms for
drug-induced pancreatitis. The most common is a hypersensi- Hydrochlorothiazide
Hydrocortisone
tivity reaction. This tends to occur 4 to 8 weeks after starting Ifosfamide
the drug and is not dose related. On rechallenge with the drug,
pancreatitis recurs within hours to days. Examples of drugs that Interferon-α
Isoniazid
may operate through this mechanism are 5-aminosalicylates, Lamivudine
metronidazole, and tetracycline. The second mechanism is the Lisinopril
presumed accumulation of a toxic metabolite that may cause pan- Losartan
creatitis, typically after several months of use. Examples of drugs Meglumine
in this category are valproic acid and didanosine (DDI). Drugs Methimazole
that induce hypertriglyceridemia (e.g., thiazides, isotretinoin, Methyldopa
tamoxifen) are also in this category. Finally, a few drugs may have Metronidazole
intrinsic toxicity wherein an overdose of them can cause pancre- 6-Mercaptopurine
atitis (erythromycin, acetaminophen). There has been significant Nelfinavir
literature in recent years about the risk of AP due to dipeptidyl Norethindrone/mestrol
peptidase-4 inhibitors, which are used with increasing frequency Pentamidine
to treat type 2 diabetes. The published reports were conflicting Pravastatin
about the risk. A recent meta-analysis of thirteen studies revealed Procainamide
a marginally higher risk of AP with DPP-4 inhibitors. However, Pyritinol
this risk was not observed in cohort studies. 106 Thus further clini- Simvastatin
cal trials are required to confirm this finding. In a population with Sulfamethazine
type 2 diabetes at high cardiovascular risk, there were numeri- Sulfamethoxazole
cally fewer events of AP among patients treated with liraglutide Stibogluconate
(a GLP-1 receptor agonist) regardless of previous history of pan- Sulindac
creatitis than in the placebo group. Liraglutide was associated, Tetracycline
however, with increases in serum lipase and amylase, which were Trimethoprim/sulfamethoxazole
not predictive of an event of subsequent AP. 107 A meta-analysis of Valproic acid
a large number of patients with type 2 diabetes revealed a nearly
2-fold increased risk of AP. 108
In general, drug-induced pancreatitis tends to be mild and *Class 1 and class 2 drugs only are listed. Class 1 drugs: 2 or more case
self-limited. The diagnosis should only be entertained after alco- reports published, absence of other causes of acute pancreatitis, rechal-
hol, gallstones, hypertriglyceridemia, hypercalcemia, and tumors lenge documented in at least 1 report. Class 2 drugs: 4 or more case
(in appropriate-aged patients) have been ruled out. Some medica- reports published, absence of other causes of acute pancreatitis, consis-
tent latency in at least 75% of cases published.
tions have been shown to cause AP in randomized trials at rela- From Badalov N, Baradarian R, Iswara K, et al. Drug induced acute pan-
tively high frequencies (e.g., 6-mercaptopurine in 3% to 5% and creatitis: an evidence based approach. Clin Gastroenterol Hepatol 2007;
didanosine in 5% to 10%), 111 but many drugs are falsely assigned 101:454-76.
causation and therefore discontinued merely because no other
cause of the AP is identified by the frustrated clinician. For some
drugs (e.g., statins), such discontinuation could prove harmful. Metabolic Disorders
Clinicians should be careful to make a diagnosis of drug-induced Hypertriglyceridemia
AP largely based on the absence of an obvious etiology and the
mere presence of 1 or a few previously published case reports. Hypertriglyceridemia is perhaps the third most common iden-
Finally, there is no evidence that any medication causes chronic tifiable cause of pancreatitis, after gallstones and alcoholism,
1
pancreatitis. accounting for anywhere from 2% to 5% to 20% of cases. A