Page 14 - Acute Pancreatitis (Viêm tụy cấp)
P. 14
CHAPTER 58 Acute Pancreatitis 905
epigastric, in the right upper quadrant, or, infrequently, confined mass may appear during the disease from a pseudocyst or a large
to the left side. Pain in the lower abdomen may arise from the inflammatory mass. 58
rapid spread of pancreatic exudation to the left colon. The general physical examination, particularly in severe pan-
Onset of pain is rapid but not as abrupt as that of a perfo- creatitis, may uncover markedly abnormal vital signs if there are
rated viscus. Usually it is at maximal intensity in 10 to 20 min- third-space fluid losses and systemic toxicity. Commonly, the
utes. Occasionally, pain gradually increases and takes several pulse is 100 to 150 beats/minute (sinus tachycardia). Blood pres-
hours to reach maximum intensity. Pain is steady and moderate sure can be initially higher than normal (perhaps due to pain) and
to very severe. There is little pain relief with changing position. then lower than normal with third-space losses and hypovolemia.
Frequently, pain is unbearable, steady, and boring. Band-like Initially the temperature may be normal, but within 1 to 3 days
radiation of the pain to the back occurs in half of patients. Pain it may increase to 101°F to 103°F, owing to the severe retro-
that lasts only a few hours and then disappears suggests a disease peritoneal inflammatory process and the release of inflammatory
other than pancreatitis, such as biliary pain or peptic ulcer. Pain mediators from the pancreas. 177
is absent in 5% to 10% of attacks, and a painless presentation may Tachypnea with shallow respirations may be present if the sub-
be a feature of serious fatal disease. 6 diaphragmatic inflammatory exudate causes painful breathing.
Ninety percent of affected patients have nausea and vomiting. Dyspnea may accompany pleural effusions, atelectasis, ARDS, or
Vomiting may be severe, may last for hours, may be accompanied heart failure. Chest examination may reveal limited diaphragmatic
by retching, and may not alleviate pain. Vomiting may be related excursion if abdominal pain causes splinting of the diaphragm, or
to severe pain or to inflammation involving the posterior gastric dullness to percussion and decreased breath sounds at the lung
wall. bases if there is a pleural effusion. There may be disorientation,
hallucinations, agitation, or coma, 178 which may be due to alcohol
Physical Examination withdrawal, hypotension, electrolyte imbalance such as hypona-
tremia, hypoxemia, fever, or toxic effects of pancreatic enzymes
Physical findings vary with the severity of an attack. Patients with on the central nervous system. Conjunctival icterus, if present,
mild pancreatitis may not appear acutely ill. Abdominal tender- may be due to choledocholithiasis (gallstone pancreatitis) or bile
ness may be mild, and abdominal guarding absent. In severe duct obstruction from edema of the head of the pancreas, or from
pancreatitis, patients look severely ill and often have abdominal coexistent liver disease.
distention, especially epigastric, which is due to gastric, small Uncommon findings in AP include panniculitis with subcu-
bowel, or colonic ileus. Almost all patients are tender in the upper taneous nodular fat necrosis that may be accompanied by poly-
abdomen, which may be elicited by gently shaking the abdomen arthritis (PPP syndrome; see Chapter 25). 179 Subcutaneous fat
or by gentle percussion. Guarding is more marked in the upper necroses are 0.5- to 2-cm tender red nodules that usually appear
abdomen. Tenderness and guarding can be less than expected, over the distal extremities but may occur over the scalp, trunk,
considering the intensity of discomfort. Abdominal rigidity, as or buttocks. They occasionally precede abdominal pain or occur
occurs in diffuse peritonitis, is unusual but can be present, and without abdominal pain, but usually they appear during a clinical
differentiation from a perforated viscus may be impossible in episode and disappear with clinical improvement.
these instances. Bowel sounds are reduced and may be absent. Some physical findings point to a specific cause of AP. Hepa-
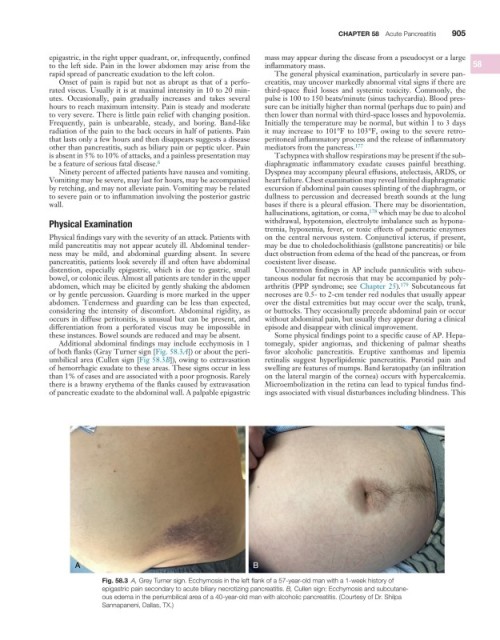
Additional abdominal findings may include ecchymosis in 1 tomegaly, spider angiomas, and thickening of palmar sheaths
of both flanks (Gray Turner sign [Fig. 58.3A]) or about the peri- favor alcoholic pancreatitis. Eruptive xanthomas and lipemia
umbilical area (Cullen sign [Fig 58.3B]), owing to extravasation retinalis suggest hyperlipidemic pancreatitis. Parotid pain and
of hemorrhagic exudate to these areas. These signs occur in less swelling are features of mumps. Band keratopathy (an infiltration
than 1% of cases and are associated with a poor prognosis. Rarely on the lateral margin of the cornea) occurs with hypercalcemia.
there is a brawny erythema of the flanks caused by extravasation Microembolization in the retina can lead to typical fundus find-
of pancreatic exudate to the abdominal wall. A palpable epigastric ings associated with visual disturbances including blindness. This
A B
Fig. 58.3 A, Grey Turner sign. Ecchymosis in the left flank of a 57-year-old man with a 1-week history of
epigastric pain secondary to acute biliary necrotizing pancreatitis. B, Cullen sign: Ecchymosis and subcutane-
ous edema in the periumbilical area of a 40-year-old man with alcoholic pancreatitis. (Courtesy of Dr. Shilpa
Sannapaneni, Dallas, TX.)