Page 17 - Acute Pancreatitis (Viêm tụy cấp)
P. 17
908 PART VII Pancreas
moderate to severe AP as protein-rich fluid extravasates from the
intravascular compartment to the peritoneal cavity. If the pan-
creas is visualized by US (bowel gas obscures the pancreas 25% to
35% of the time), it is usually diffusely enlarged and hypoechoic.
Less frequently, there are focal hypoechoic areas. There also may G
be US evidence of chronic pancreatitis, such as intraductal or
parenchymal calcification(s) and dilation of the PD. US is not a
good imaging test to evaluate extrapancreatic spread of pancreatic P
inflammation or pancreatic necrosis and consequently is not use-
ful to ascertain severity of pancreatitis. During the course of AP,
US can be used to evaluate progression of a pseudocyst (discussed
later). Owing to overlying gas, the diagnosis of cholelithiasis may
be obscured during the acute attack but may be found after bowel
gas has receded. Contrast-enhanced US of the pancreas may be
useful in the future to assess the severity of AP. 207
EUS and ERCP
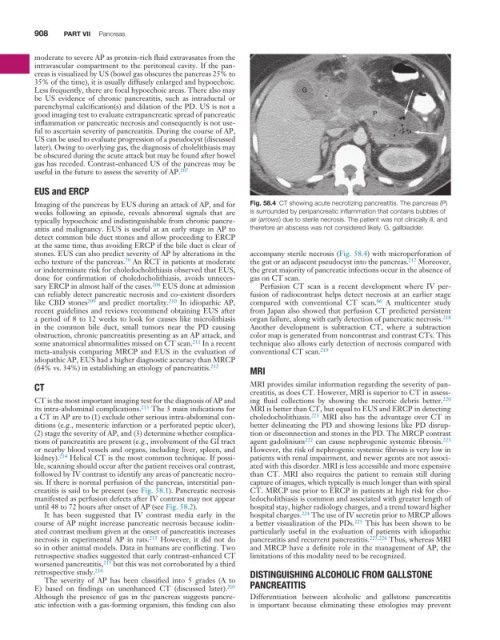
Imaging of the pancreas by EUS during an attack of AP, and for Fig. 58.4 CT showing acute necrotizing pancreatitis. The pancreas (P)
weeks following an episode, reveals abnormal signals that are is surrounded by peripancreatic inflammation that contains bubbles of
typically hypoechoic and indistinguishable from chronic pancre- air (arrows) due to sterile necrosis. The patient was not clinically ill, and
atitis and malignancy. EUS is useful at an early stage in AP to therefore an abscess was not considered likely. G, gallbladder.
detect common bile duct stones and allow proceeding to ERCP
at the same time, thus avoiding ERCP if the bile duct is clear of
stones. EUS can also predict severity of AP by alterations in the accompany sterile necrosis (Fig. 58.4) with microperforation of
79
echo texture of the pancreas. An RCT in patients at moderate the gut or an adjacent pseudocyst into the pancreas. 217 Moreover,
or indeterminate risk for choledocholithiasis observed that EUS, the great majority of pancreatic infections occur in the absence of
done for confirmation of choledocholithiasis, avoids unneces- gas on CT scan.
sary ERCP in almost half of the cases. 208 EUS done at admission Perfusion CT scan is a recent development where IV per-
can reliably detect pancreatic necrosis and co-existent disorders fusion of radiocontrast helps detect necrosis at an earlier stage
86
like CBD stones 209 and predict mortality. 210 In idiopathic AP, compared with conventional CT scan. A multicenter study
recent guidelines and reviews recommend obtaining EUS after from Japan also showed that perfusion CT predicted persistent
a period of 8 to 12 weeks to look for causes like microlithiasis organ failure, along with early detection of pancreatic necrosis. 218
in the common bile duct, small tumors near the PD causing Another development is subtraction CT, where a subtraction
obstruction, chronic pancreatitis presenting as an AP attack, and color map is generated from noncontrast and contrast CTs. This
some anatomical abnormalities missed on CT scan. 211 In a recent technique also allows early detection of necrosis compared with
meta-analysis comparing MRCP and EUS in the evaluation of conventional CT scan. 219
idiopathic AP, EUS had a higher diagnostic accuracy than MRCP
(64% vs. 34%) in establishing an etiology of pancreatitis. 212 MRI
CT MRI provides similar information regarding the severity of pan-
creatitis, as does CT. However, MRI is superior to CT in assess-
CT is the most important imaging test for the diagnosis of AP and ing fluid collections by showing the necrotic debris better. 220
its intra-abdominal complications. 213 The 3 main indications for MRI is better than CT, but equal to EUS and ERCP in detecting
a CT in AP are to (1) exclude other serious intra-abdominal con- choledocholithiasis. 221 MRI also has the advantage over CT in
ditions (e.g., mesenteric infarction or a perforated peptic ulcer), better delineating the PD and showing lesions like PD disrup-
(2) stage the severity of AP, and (3) determine whether complica- tion or disconnection and stones in the PD. The MRCP contrast
tions of pancreatitis are present (e.g., involvement of the GI tract agent gadolinium 222 can cause nephrogenic systemic fibrosis. 223
or nearby blood vessels and organs, including liver, spleen, and However, the risk of nephrogenic systemic fibrosis is very low in
kidney). 214 Helical CT is the most common technique. If possi- patients with renal impairment, and newer agents are not associ-
ble, scanning should occur after the patient receives oral contrast, ated with this disorder. MRI is less accessible and more expensive
followed by IV contrast to identify any areas of pancreatic necro- than CT. MRI also requires the patient to remain still during
sis. If there is normal perfusion of the pancreas, interstitial pan- capture of images, which typically is much longer than with spiral
creatitis is said to be present (see Fig. 58.1). Pancreatic necrosis CT. MRCP use prior to ERCP in patients at high risk for cho-
manifested as perfusion defects after IV contrast may not appear ledocholithiasis is common and associated with greater length of
until 48 to 72 hours after onset of AP (see Fig. 58.2). hospital stay, higher radiology charges, and a trend toward higher
It has been suggested that IV contrast media early in the hospital charges. 224 The use of IV secretin prior to MRCP allows
course of AP might increase pancreatic necrosis because iodin- a better visualization of the PDs. 225 This has been shown to be
ated contrast medium given at the onset of pancreatitis increases particularly useful in the evaluation of patients with idiopathic
necrosis in experimental AP in rats. 215 However, it did not do pancreatitis and recurrent pancreatitis. 225,226 Thus, whereas MRI
so in other animal models. Data in humans are conflicting. Two and MRCP have a definite role in the management of AP, the
retrospective studies suggested that early contrast-enhanced CT limitations of this modality need to be recognized.
worsened pancreatitis, 215 but this was not corroborated by a third
retrospective study. 216 DISTINGUISHING ALCOHOLIC FROM GALLSTONE
The severity of AP has been classified into 5 grades (A to
E) based on findings on unenhanced CT (discussed later). 203 PANCREATITIS
Although the presence of gas in the pancreas suggests pancre- Differentiation between alcoholic and gallstone pancreatitis
atic infection with a gas-forming organism, this finding can also is important because eliminating these etiologies may prevent