Page 13 - Vasoclick emagazine Issue2
P. 13
Had an exposure group that had patients with
This review and meta-analysis followed the
psoriasis and a non-exposure group that had
Meta-analysis of Observational Studies in
patients without psoriasis.
Epidemiology (MOOSE) reporting guideline
4
Reported the risk estimates of VTE and/or
group19 and the Preferred Reporting Items for
PVD.
Meta-analyses
and
Systematic
Studies with confirmed clinical diagnoses of
(PRISMA) reporting 2020 guideline.
5
psoriasis, VTE, and PVD.
Data Sources:
Studies excluded:
MEDLINE, Embase, Cochrane Library, Web of
Cross-sectional studies, case-control studies,
Science, and the Cumulative Index to Nursing
case reports, editorials, review articles, and
and Allied Health Literature were searched for
nonhuman studies were excluded.
publications that studied the associations of
2
psoriasis with VTE or PVD from their
Data Extraction:
respective inception to May 21, 2021.
2
First author, year of publication, country,
database, study period, patient characteristics
Study Selection Criteria:
(sample size, mean age, and sex), definition of
studies
Cohort
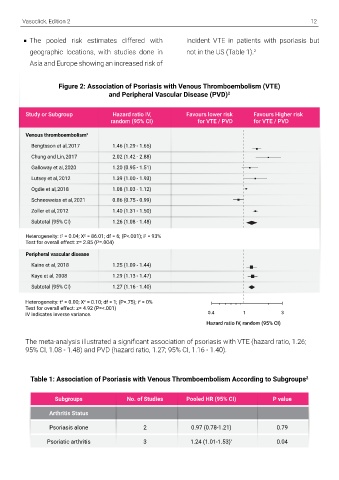
Vasoclick, Edition 2 12 Methods: Reviews that examined the associations of psoriasis with VTE or PVD.
psoriasis, and outcomes of interest (VTE and There were 9 (69.2%) studies that reported The pooled risk estimates differed with incident VTE in patients with psoriasis but
PVD). 2 HR or SIR and were selected for quantitative geographic locations, with studies done in not in the US (Table 1).
2
The adjusted risk estimates, including hazard meta-analysis (Figure 1). Asia and Europe showing an increased risk of
ratios (HRs), risk ratios (RRs), and
standardized incidence ratios (SIRs), with 95% Figure 2: Association of Psoriasis with Venous Thromboembolism (VTE)
confidence intervals (CIs). 2 and Peripheral Vascular Disease (PVD) 2
Study or Subgroup Hazard ratio IV, Favours lower risk Favours Higher risk
Data Synthesis: random (95% CI) for VTE / PVD for VTE / PVD
The meta-analyses were conducted using Venous thromboembolism 2
Review Manager version 5.4.1 (The Cochrane Bengtsson et al,2017 1.46 (1.29 - 1.65)
Collaboration), and Stata, version 17 Chung and Lin,2017 2.02 (1.42 - 2.88)
(StataCorp). A P value of <0.05 was defined as Galloway et al,2020 1.20 (0.95 - 1.51)
statistically significant. 2 Lutsey et al,2012 1.39 (1.00 - 1.93)
HRs and SIRs were used for meta-analysis to Ogdie et al,2018 1.08 (1.03 - 1.12)
analyse risk for the entire study period. The Schneeweiss et al,2021 0.86 (0.75 - 0.99)
adjusted risk estimates of subgroups were Zoller et al,2012 1.40 (1.31 - 1.50)
pooled when overall effects were not Subtotal (95% CI) 1.26 (1.08 - 1.48)
available. 2 Heterogeneity: t = 0.04; X = 86.01; df = 6; (P<.001); i = 93%
2
2
2
Crude risk estimates with 95% CI were Test for overall effect: z= 2.85 (P=.004)
calculated when not available in the studies. 2 Peripheral vascular disease
I statistic was used to quantify between-study Risk for Incident VTE: Kaine et al, 2018 1.25 (1.09 - 1.44)
2
Kaye et al, 2008 1.29 (1.13 - 1.47)
heterogeneity with I >50% indicating moderate Based on the 9 studies (12,052,781
2
heterogeneity. 2 participants) examined, patients with Subtotal (95% CI) 1.27 (1.16 - 1.40)
2
2
2
psoriasis had a 1.26-fold increased risk for Heterogeneity: t = 0.00; X = 0.10; df = 1; (P=.75); i = 0%
Test for overall effect: z= 4.92 (P=<.001)
Results: incident VTE than those without psoriasis IV indicates inverse variance. 0.4 1 3
Study Selection and their characteris- (pooled HR, 1.26; 95%, CI 1.08-1.48; I = 93%) Hazard ratio IV, random (95% CI)
2
tics: (Figure 2). 2 The meta-analysis illustrated a significant association of psoriasis with VTE (hazard ratio, 1.26;
A total of 1836 records were retrieved from 95% CI, 1.08 - 1.48) and PVD (hazard ratio, 1.27; 95% CI, 1.16 - 1.40).
the literature search, 13 cohort studies The association remained significant in
(12,435,982 participants) out of which were patients with psoriatic arthritis but did not Table 1: Association of Psoriasis with Venous Thromboembolism According to Subgroups 2
selected for qualitative review (Figure 1). increase significantly in patients with
psoriasis alone (Table 1). 2
Subgroups No. of Studies Pooled HR (95% CI) P value
Out of the 13 studies selected, 9 (69.2%)
reported the risk estimates of incident VTE, The studies done on women showed an Arthritis Status
and 4 (30.8%) reported the risk estimates of increased risk for VTE as opposed to those Psoriasis alone 2 0.97 (0.78-1.21) 0.79
incident PVD (Figure 1). done on men(Table 1). 2 Psoriatic arthritis 3 1.24 (1.01-1.53) 0.04
*