Page 12 - Risk Reduction Series - Documentation Essentials (Part One)
P. 12
SVMIC Risk Reduction Series: Documentation Essentials
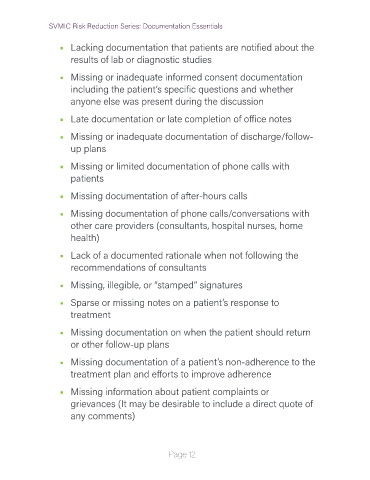
• Lacking documentation that patients are notified about the
results of lab or diagnostic studies
• Missing or inadequate informed consent documentation
including the patient’s specific questions and whether
anyone else was present during the discussion
• Late documentation or late completion of office notes
• Missing or inadequate documentation of discharge/follow-
up plans
• Missing or limited documentation of phone calls with
patients
• Missing documentation of after-hours calls
• Missing documentation of phone calls/conversations with
other care providers (consultants, hospital nurses, home
health)
• Lack of a documented rationale when not following the
recommendations of consultants
• Missing, illegible, or “stamped” signatures
• Sparse or missing notes on a patient’s response to
treatment
• Missing documentation on when the patient should return
or other follow-up plans
• Missing documentation of a patient’s non-adherence to the
treatment plan and efforts to improve adherence
• Missing information about patient complaints or
grievances (It may be desirable to include a direct quote of
any comments)
Page 12