Page 17 - Risk Reduction Series - Documentation Essentials (Part One)
P. 17
SVMIC Risk Reduction Series: Documentation Essentials
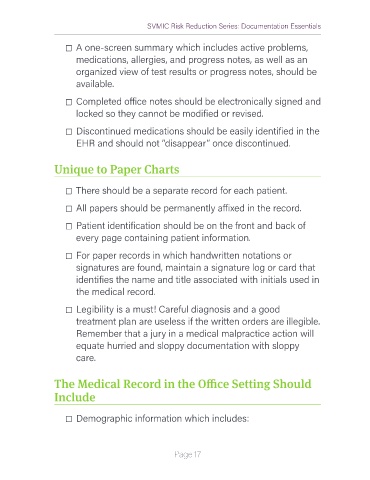
☐ A one-screen summary which includes active problems,
medications, allergies, and progress notes, as well as an
organized view of test results or progress notes, should be
available.
☐ Completed office notes should be electronically signed and
locked so they cannot be modified or revised.
☐ Discontinued medications should be easily identified in the
EHR and should not “disappear” once discontinued.
Unique to Paper Charts
☐ There should be a separate record for each patient.
☐ All papers should be permanently affixed in the record.
☐ Patient identification should be on the front and back of
every page containing patient information.
☐ For paper records in which handwritten notations or
signatures are found, maintain a signature log or card that
identifies the name and title associated with initials used in
the medical record.
☐ Legibility is a must! Careful diagnosis and a good
treatment plan are useless if the written orders are illegible.
Remember that a jury in a medical malpractice action will
equate hurried and sloppy documentation with sloppy
care.
The Medical Record in the Office Setting Should
Include
☐ Demographic information which includes:
Page 17