Page 81 - QCS.19 SPD - PPO
P. 81
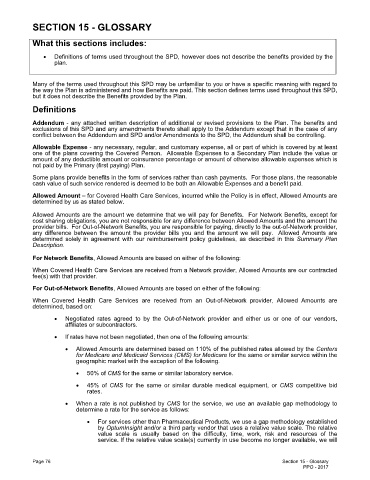
SECTION 15 - GLOSSARY
What this sections includes:
· Definitions of terms used throughout the SPD, however does not describe the benefits provided by the
plan.
Many of the terms used throughout this SPD may be unfamiliar to you or have a specific meaning with regard to
the way the Plan is administered and how Benefits are paid. This section defines terms used throughout this SPD,
but it does not describe the Benefits provided by the Plan.
Definitions
Addendum - any attached written description of additional or revised provisions to the Plan. The benefits and
exclusions of this SPD and any amendments thereto shall apply to the Addendum except that in the case of any
conflict between the Addendum and SPD and/or Amendments to the SPD, the Addendum shall be controlling.
Allowable Expense - any necessary, regular, and customary expense, all or part of which is covered by at least
one of the plans covering the Covered Person. Allowable Expenses to a Secondary Plan include the value or
amount of any deductible amount or coinsurance percentage or amount of otherwise allowable expenses which is
not paid by the Primary (first paying) Plan.
Some plans provide benefits in the form of services rather than cash payments. For those plans, the reasonable
cash value of such service rendered is deemed to be both an Allowable Expenses and a benefit paid.
Allowed Amount – for Covered Health Care Services, incurred while the Policy is in effect, Allowed Amounts are
determined by us as stated below.
Allowed Amounts are the amount we determine that we will pay for Benefits. For Network Benefits, except for
cost sharing obligations, you are not responsible for any difference between Allowed Amounts and the amount the
provider bills. For Out-of-Network Benefits, you are responsible for paying, directly to the out-of-Network provider,
any difference between the amount the provider bills you and the amount we will pay. Allowed Amounts are
determined solely in agreement with our reimbursement policy guidelines, as described in this Summary Plan
Description.
For Network Benefits, Allowed Amounts are based on either of the following:
When Covered Health Care Services are received from a Network provider, Allowed Amounts are our contracted
fee(s) with that provider.
For Out-of-Network Benefits, Allowed Amounts are based on either of the following:
When Covered Health Care Services are received from an Out-of-Network provider, Allowed Amounts are
determined, based on:
· Negotiated rates agreed to by the Out-of-Network provider and either us or one of our vendors,
affiliates or subcontractors.
· If rates have not been negotiated, then one of the following amounts:
· Allowed Amounts are determined based on 110% of the published rates allowed by the Centers
for Medicare and Medicaid Services (CMS) for Medicare for the same or similar service within the
geographic market with the exception of the following.
· 50% of CMS for the same or similar laboratory service.
· 45% of CMS for the same or similar durable medical equipment, or CMS competitive bid
rates.
· When a rate is not published by CMS for the service, we use an available gap methodology to
determine a rate for the service as follows:
· For services other than Pharmaceutical Products, we use a gap methodology established
by OptumInsight and/or a third party vendor that uses a relative value scale. The relative
value scale is usually based on the difficulty, time, work, risk and resources of the
service. If the relative value scale(s) currently in use become no longer available, we will
Page 76 Section 15 - Glossary
PPO - 2017