Page 12 - QCHC.19 Employee Benefits
P. 12
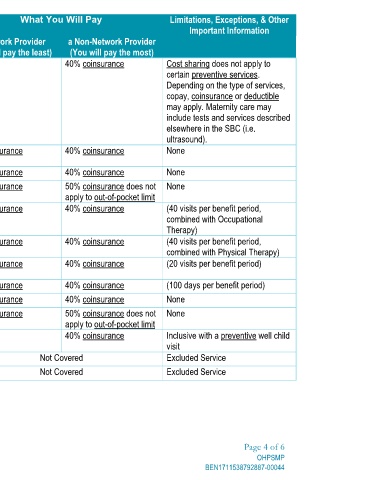
Limitations, Exceptions, & Other
Important Information Cost sharing does not apply to certain preventive services. Depending on the type of services, copay, coinsurance or deductible may apply. Maternity care may include tests and services described elsewhere in the SBC (i.e. ultrasound). None None None (40 visits per benefit period, combined with Occupational Therapy) (40 visits per benefit period, combined with Physical Therapy) (20 visits per benefit period) (100 days per benefit period) None None Inclusive with a preventive well child visit Excluded Service Excluded Service Page 4 of 6 OHPSMP BEN1711538792887-00044
a Non-Network Provider (You will pay the most) 40% coinsurance 40% coinsurance 40% coinsurance 50% coinsurance does not apply to out-of-pocket limit 40% coinsurance 40% coinsurance 40% coinsurance 40% coinsurance 40% coinsurance 50% coinsurance does not apply to out-of-pocket limit 40% coinsurance
What You Will Pay Not Covered Not Covered
a Network Provider (You will pay the least) No charge 20% coinsurance 20% coinsurance 20% coinsurance 20% coinsurance 20% coinsurance 20% coinsurance 20% coinsurance 20% coinsurance 20% coinsurance No charge
Services You May Need Office visits Childbirth/delivery professional services Childbirth/delivery facility services Home health care Rehabilitation services (Physical Therapy) Habilitation services (Occupational Therapy) Habilitation services (Speech Therapy) Skilled nursing care Durable medical equipment Hospice services Children's eye exam Children's glasses Children's dental check-up
Common Medical Event If you are pregnant If you need help recovering or have other special health needs If your child needs dental or eye care