Page 6 - MAC.Solution.Brochure-FlipPDF_Neat
P. 6
Why to Say, “No to Pneumatic.” Warning Signs with
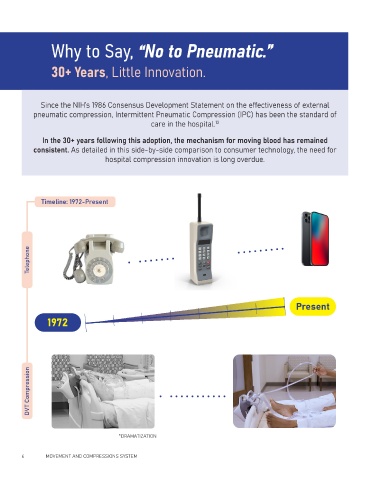
30+ Years, Little Innovation. Pneumatic Compression
The pneumatic mechanism of action for compressing the leg has caused an
Since the NIH’s 1986 Consensus Development Statement on the effectiveness of external array of complications for both patients and hospital staff. According to a 2018
pneumatic compression, Intermittent Pneumatic Compression (IPC) has been the standard of study on staff and patient perspectives with mechanical prophylaxis for venous
care in the hospital. 13 thromboembolism - the most significant barrier to noncompliance was patient
discomfort with sleep interference.
11
In the 30+ years following this adoption, the mechanism for moving blood has remained
consistent. As detailed in this side-by-side comparison to consumer technology, the need for
hospital compression innovation is long overdue.
Other challenges can include but
are not limited to the following:
PATIENT
Timeline: 1972-Present DISCOMFORT
• Fall Risk 12 to 16
• Patient Tethered HOURS
Telephone • Aerosolization of
• Skin Breakdown Risk
• Sleep Disruption *average per 24hr period (16)
• Cumbersome Pump
Present
1972
Workflow Challenges
DVT Compression Patient dissatisfaction has compounding effects on
care providers. The need to constantly reconnect
tubing and reposition sleeves on IPC devices can
take valuable time and effort away from other
critical duties in the hospital. Caregiver overload
can affect key hospital measures such as
HCAHPS Surveys which rely on patient
*DRAMATIZATION satisfaction and quality of care.
6 MOVEMENT AND COMPRESSIONS SYSTEM MOVEMENT AND COMPRESSIONS SYSTEM 7
MOVEMENT AND COMPRESSIONS SYSTEM 7