Page 39 - Feline Cardiology
P. 39
32 Section A: Clinical Entities
Clinical Entities
A
B
C
D
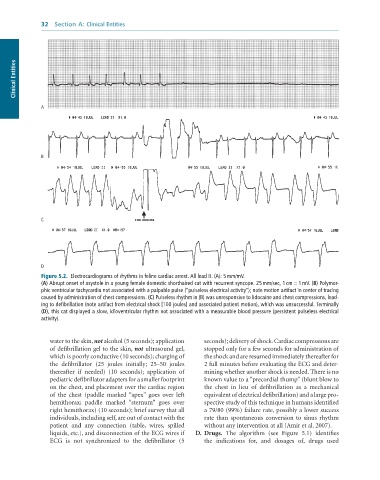
Figure 5.2. Electrocardiograms of rhythms in feline cardiac arrest. All lead II. (A): 5 mm/mV.
(A) Abrupt onset of asystole in a young female domestic shorthaired cat with recurrent syncope. 25 mm/sec, 1 cm = 1 mV. (B) Polymor-
phic ventricular tachycardia not associated with a palpable pulse (“pulseless electrical activity”); note motion artifact in center of tracing
caused by administration of chest compressions. (C) Pulseless rhythm in (B) was unresponsive to lidocaine and chest compressions, lead-
ing to defibrillation (note artifact from electrical shock [100 joules] and associated patient motion), which was unsuccessful. Terminally
(D), this cat displayed a slow, idioventricular rhythm not associated with a measurable blood pressure (persistent pulseless electrical
activity).
water to the skin, not alcohol (5 seconds); application seconds); delivery of shock. Cardiac compressions are
of defibrillation gel to the skin, not ultrasound gel, stopped only for a few seconds for administration of
which is poorly conductive (10 seconds); charging of the shock and are resumed immediately thereafter for
the defibrillator (25 joules initially; 25–50 joules 2 full minutes before evaluating the ECG and deter-
thereafter if needed) (10 seconds); application of mining whether another shock is needed. There is no
pediatric defibrillator adapters for a smaller footprint known value to a “precordial thump” (blunt blow to
on the chest, and placement over the cardiac region the chest in lieu of defibrillation as a mechanical
of the chest (paddle marked “apex” goes over left equivalent of electrical defibrillation) and a large pro-
hemithorax; paddle marked “sternum” goes over spective study of this technique in humans identified
right hemithorax) (10 seconds); brief survey that all a 79/80 (99%) failure rate, possibly a lower success
individuals, including self, are out of contact with the rate than spontaneous conversion to sinus rhythm
patient and any connection (table, wires, spilled without any intervention at all (Amir et al. 2007).
liquids, etc.), and disconnection of the ECG wires if D. Drugs. The algorithm (see Figure 5.1) identifies
ECG is not synchronized to the defibrillator (5 the indications for, and dosages of, drugs used