Page 849 - Small Animal Internal Medicine, 6th Edition
P. 849
CHAPTER 49 Disorders of the Endocrine Pancreas 821
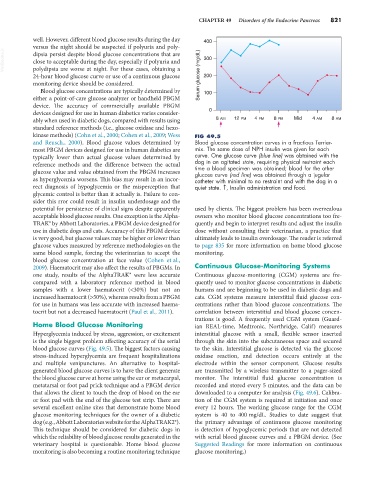
well. However, different blood glucose results during the day 400
versus the night should be suspected if polyuria and poly-
VetBooks.ir dipsia persist despite blood glucose concentrations that are 300
close to acceptable during the day, especially if polyuria and
polydipsia are worse at night. For these cases, obtaining a
24-hour blood glucose curve or use of a continuous glucose Serum glucose (mg/dL) 200
monitoring device should be considered.
Blood glucose concentrations are typically determined by 100
either a point-of-care glucose analyzer or handheld PBGM
device. The accuracy of commercially available PBGM
devices designed for use in human diabetics varies consider- 0
ably when used in diabetic dogs, compared with results using 8 AM 12 PM 4 PM 8 PM Mid 4 AM 8 AM
standard reference methods (i.e., glucose oxidase and hexo-
kinase methods) (Cohn et al., 2000; Cohen et al., 2009; Wess FIG 49.5
and Reusch., 2000). Blood glucose values determined by Blood glucose concentration curves in a fractious Terrier-
most PBGM devices designed for use in human diabetics are mix. The same dose of NPH insulin was given for each
typically lower than actual glucose values determined by curve. One glucose curve (blue line) was obtained with the
reference methods and the difference between the actual dog in an agitated state, requiring physical restraint each
time a blood specimen was obtained; blood for the other
glucose value and value obtained from the PBGM increases glucose curve (red line) was obtained through a jugular
as hyperglycemia worsens. This bias may result in an incor- catheter with minimal to no restraint and with the dog in a
rect diagnosis of hypoglycemia or the misperception that quiet state. ↑, Insulin administration and food.
glycemic control is better than it actually is. Failure to con-
sider this rror could result in insulin underdosage and the
potential for persistence of clinical signs despite apparently used by clients. The biggest problem has been overzealous
acceptable blood glucose results. One exception is the Alpha- owners who monitor blood glucose concentrations too fre-
TRAK® by Abbott Laboratories, a PBGM device designed for quently and begin to interpret results and adjust the insulin
use in diabetic dogs and cats. Accuracy of this PBGM device dose without consulting their veterinarian, a practice that
is very good, but glucose values may be higher or lower than ultimately leads to insulin overdosage. The reader is referred
glucose values measured by reference methodologies on the to page 835 for more information on home blood glucose
same blood sample, forcing the veterinarian to accept the monitoring.
blood glucose concentration at face value (Cohen et al.,
2009). Haematocrit may also affect the results of PBGMs. In Continuous Glucose-Monitoring Systems
one study, results of the AlphaTRAK® were less accurate Continuous glucose-monitoring (CGM) systems are fre-
compared with a laboratory reference method in blood quently used to monitor glucose concentrations in diabetic
samples with a lower haematocrit (<30%) but not an humans and are beginning to be used in diabetic dogs and
increased haematocrit (>50%), whereas results from a PBGM cats. CGM systems measure interstitial fluid glucose con-
for use in humans was less accurate with increased haema- centrations rather than blood glucose concentrations. The
tocrit but not a decreased haematocrit (Paul et al., 2011). correlation between interstitial and blood glucose concen-
trations is good. A frequently used CGM system (Guard-
Home Blood Glucose Monitoring ian REAL-time, Medtronic, Northridge, Calif) measures
Hyperglycemia induced by stress, aggression, or excitement interstitial glucose with a small, flexible sensor inserted
is the single biggest problem affecting accuracy of the serial through the skin into the subcutaneous space and secured
blood glucose curves (Fig. 49.5). The biggest factors causing to the skin. Interstitial glucose is detected via the glucose
stress-induced hyperglycemia are frequent hospitalizations oxidase reaction, and detection occurs entirely at the
and multiple venipunctures. An alternative to hospital- electrode within the sensor component. Glucose results
generated blood glucose curves is to have the client generate are transmitted by a wireless transmitter to a pager-sized
the blood glucose curve at home using the ear or metacarpal, monitor. The interstitial fluid glucose concentration is
metatarsal or foot pad prick technique and a PBGM device recorded and stored every 5 minutes, and the data can be
that allows the client to touch the drop of blood on the ear downloaded to a computer for analysis (Fig. 49.6). Calibra-
or foot pad with the end of the glucose test strip. There are tion of the CGM system is required at initiation and once
several excellent online sites that demonstrate home blood every 12 hours. The working glucose range for the CGM
glucose monitoring techniques for the owner of a diabetic system is 40 to 400 mg/dL. Studies to date suggest that
dog (e.g., Abbott Laboratories website for the AlphaTRAK2®). the primary advantage of continuous glucose monitoring
This technique should be considered for diabetic dogs in is detection of hypoglycemic periods that are not detected
which the reliability of blood glucose results generated in the with serial blood glucose curves and a PBGM device. (See
veterinary hospital is questionable. Home blood glucose Suggested Readings for more information on continuous
monitoring is also becoming a routine monitoring technique glucose monitoring.)