Page 245 - Manual of Equine Field Surgery
P. 245
Rectovagina Fistula Repair 241
l
Sutures are positioned approximately 1 cm apart,
avoiding the vaginal and rectal mucosa. Once the
cranial half of the rectovaginal shelf is recon-
structed, closure of the vaginal mucosa is corn-
pleted, followed by closure of the remaining
caudal half of the rectovaginal shelf. The trans-
verse perinea! skin incision is closed with No. 2-0
nonabsorbable suture using a simple interrupted
pattern. If indicated, Caslick's procedure is per-
formed to appose the vulvar opening.
Klug Technique
Fistulas up to 6 cm have been repaired using this
7
technique. The Klug technique provides good
visualization, a durable and stable closure, and
good first-time healing success rate without dis-
rupting the integrity of the anal sphincter. Repair-
ing a large fistula using this technique should be
attempted with caution. Tissue mobilization is A
difficult in large fistula repairs and may require an -
alternative repair method. Cranially located fistu-
las should not be repaired with this technique ·=::_ )
because of inadequate visualization and limited
working room. B
Beginning at the caudal edge of the fistula, an
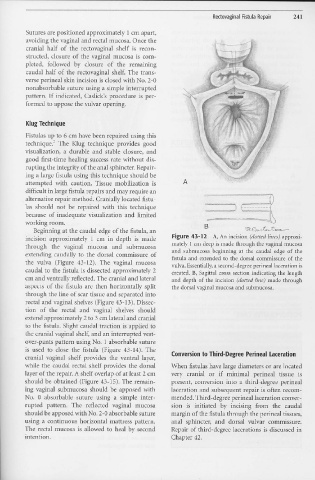
incision approximately 1 cm in depth is made Figure 43-12 A, An incision ( dotted lines) approxi-
through the vaginal mucosa and subrnucosa mately 1 cm deep is made through the vaginal mucosa
and submucosa beginning at the caudal edge of the
extending caudally to the dorsal cornmissure of fistula and extended to the dorsal commissure of the
the vulva (Figure 43-12). The vaginal mucosa vulva. Essentially, a second-degree perineal laceration is
caudal to the fistula is dissected approximately 2 created. B, Sagittal cross section indicating the length
cm and ventrally reflected. The cranial and lateral and depth of the incision (dotted line) made through
aspects of the fistula are then horizontally split the dorsal vaginal mucosa and submucosa.
through the line of scar tissue and separated into
rectal and vaginal shelves (Figure 43-13 ). Dissec-
tion of the rectal and vaginal shelves should
extend approximately 2 to 3 cm lateral and cranial
to the fistula. Slight caudal traction is applied to
the cranial vaginal shelf, and an interrupted vest-
over-pants pattern using No. 1 absorbable suture
is used to close the fistula (Figure 43-14). The Conversion to Third-Degree Perineal Laceration
cranial vaginal shelf provides the ventral layer,
while the caudal rectal shelf provides the dorsal When fistulas have large diameters or are located
layer of the repair. A shelf overlap of at least 2 cm very cranial or if minimal perineal tissue is
should be obtained (Figure 43-15). The remain- present, conversion into a third-degree perinea!
ing vaginal submucosa should be apposed with laceration and subsequent repair is often recom-
No. 0 absorbable suture 11siI1g a simple inter- mended.Third-degree perineal laceration conver-
rupted pattern. The reflected vaginal mucosa sion is initiated by incising from the caudal
should be apposed with No. 2-0 absorbable suture margin of the fistula through the perineal tissues,
using a continuous horizontal mattress pattern. anal sphincter, and dorsal vulvar commissure.
The rectal mucosa is allowed to heal by second Repair of third-degree lacerations is discussed in
intention. Chapter 42.