Page 19 - HPB Handbook - May 30 2022 (Flipbook) v2
P. 19
Page 19 of 22
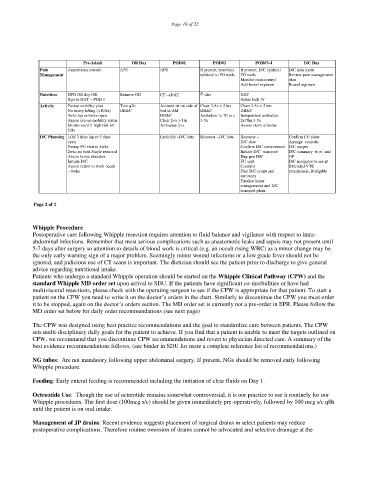
Pre-Admit OR Day POD#1 POD#2 POD#3-4 D/C Day
m
in
pa
D/C
Pain Anaesthesia consult APS APS If present, transition If present, D/C epidural
e
ds
Management epidural to PO meds PO meds Review pain management
Monitor pain control plan
Add bowel regimen Bowel regimen
Nutrition NPO OR day OR Remove OG CF DAT diet DAT
Sips to DAT ~ POD 1 Saline lock IV
-
3
>
5
x
C
ir
h
a
hr
2
s
C
h
a
o
f
5
x
-
ir
3
de
s
ted
s
i
A
s
s
s
i
n
i
t
o
hr
2
s
>
Activity Postop mobility plan Turn q2h
DB
DB
No heavy lifting (<10lbs) DB&C bed in AM
&C
&C
m
A
te
b
4wks lap or 6wks open DB&C x Independent ambulate:
m
1
x
70
ul
a
5x
Assess pre-op mobility status Chair 2+x > 1hr 2x70m 3-5x
3
-
Inform ward if high risk for Ambulate 2+x Assess stairs at home
falls
D/C Planning LOS 3 days lap or 5 days Establish ~D/C date Reassess ~D/C date Reassess ~ Confirm FU plans
ult
e
ng
s
n
o
c
s
Ar
a
r
open D/C date
i
pts
r
Postop FU visit in 4wks Confirm D/C environment
D/C
s
c
2wks no bath Staple removal Initiate D/C transport D/C summary to pt and
Assess home situation Day pre D/C GP
Initiate D/C FU appt D/C navigator to see pt
Assess return to work needs Consults Extended VTE
~ 6wks Prep D/C script and prophylaxis, if eligible
summary
Finalize home
arrangements and D/C
transport plans
Page 2 of 2
Whipple Procedure
Postoperative care following Whipple resection requires attention to fluid balance and vigilance with respect to intra-
abdominal infections. Remember that most serious complications such as anastomotic leaks and sepsis may not present until
5-7 days after surgery so attention to details of blood work is critical (e.g. an occult rising WBC) as a minor change may be
the only early warning sign of a major problem. Seemingly minor wound infections or a low grade fever should not be
ignored, and judicious use of CT scans is important. The dietician should see the patient prior to discharge to give general
advice regarding nutritional intake.
Patients who undergo a standard Whipple operation should be started on the Whipple Clinical Pathway (CPW) and the
standard Whipple MD order set upon arrival to SDU. If the patients have significant co-morbidities or have had
multivisceral resections, please check with the operating surgeon to see if the CPW is appropriate for that patient. To start a
patient on the CPW you need to write it on the doctor’s orders in the chart. Similarly to discontinue the CPW you must order
it to be stopped, again on the doctor’s orders section. The MD order set is currently not a pre-order in EPR. Please follow the
MD order set below for daily order recommendations (see next page)
The CPW was designed using best practice recommendations and the goal to standardize care between patients. The CPW
sets multi-disciplinary daily goals for the patient to achieve. If you find that a patient is unable to meet the targets outlined on
CPW, we recommend that you discontinue CPW recommendations and revert to physician directed care. A summary of the
best evidence recommendations follows, (see binder in SDU for more a complete reference list of recommendations.)
NG tubes: Are not mandatory following upper abdominal surgery. If present, NGs should be removed early following
Whipple procedure.
Feeding: Early enteral feeding is recommended including the initiation of clear fluids on Day 1.
Octreotide Use: Though the use of octreotide remains somewhat controversial, it is our practice to use it routinely for our
Whipple procedures. The first dose (100mcg s/c) should be given immediately pre-operatively, followed by 100 mcg s/c q8h
until the patient is on oral intake.
Management of JP drains: Recent evidence suggests placement of surgical drains in select patients may reduce
postoperative complications. Therefore routine omission of drains cannot be advocated and selective drainage at the