Page 385 - Libro 2
P. 385
23 — Evaluation of Kidney and Liver Transplants
365
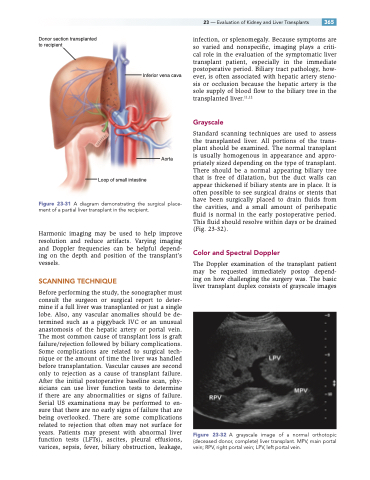
Donor section transplanted to recipient
infection, or splenomegaly. Because symptoms are so varied and nonspecific, imaging plays a criti- cal role in the evaluation of the symptomatic liver transplant patient, especially in the immediate postoperative period. Biliary tract pathology, how- ever, is often associated with hepatic artery steno- sis or occlusion because the hepatic artery is the sole supply of blood flow to the biliary tree in the transplanted liver.11,12
Grayscale
Standard scanning techniques are used to assess the transplanted liver. All portions of the trans- plant should be examined. The normal transplant is usually homogenous in appearance and appro- priately sized depending on the type of transplant. There should be a normal appearing biliary tree that is free of dilatation, but the duct walls can appear thickened if biliary stents are in place. It is often possible to see surgical drains or stents that have been surgically placed to drain fluids from the cavities, and a small amount of perihepatic fluid is normal in the early postoperative period. This fluid should resolve within days or be drained (Fig. 23-32).
Color and Spectral Doppler
The Doppler examination of the transplant patient may be requested immediately postop depend- ing on how challenging the surgery was. The basic liver transplant duplex consists of grayscale images
Figure 23-32 A grayscale image of a normal orthotopic (deceased donor, complete) liver transplant. MPV, main portal vein; RPV, right portal vein; LPV, left portal vein.
Inferior vena cava
Aorta
Loop of small intestine
Figure 23-31 A diagram demonstrating the surgical place- ment of a partial liver transplant in the recipient.
Harmonic imaging may be used to help improve resolution and reduce artifacts. Varying imaging and Doppler frequencies can be helpful depend- ing on the depth and position of the transplant’s vessels.
SCANNING TECHNIQUE
Before performing the study, the sonographer must consult the surgeon or surgical report to deter- mine if a full liver was transplanted or just a single lobe. Also, any vascular anomalies should be de- termined such as a piggyback IVC or an unusual anastomosis of the hepatic artery or portal vein. The most common cause of transplant loss is graft failure/rejection followed by biliary complications. Some complications are related to surgical tech- nique or the amount of time the liver was handled before transplantation. Vascular causes are second only to rejection as a cause of transplant failure. After the initial postoperative baseline scan, phy- sicians can use liver function tests to determine if there are any abnormalities or signs of failure. Serial US examinations may be performed to en- sure that there are no early signs of failure that are being overlooked. There are some complications related to rejection that often may not surface for years. Patients may present with abnormal liver function tests (LFTs), ascites, pleural effusions, varices, sepsis, fever, biliary obstruction, leakage,