Page 14 - Digital Medicaid Workbook
P. 14
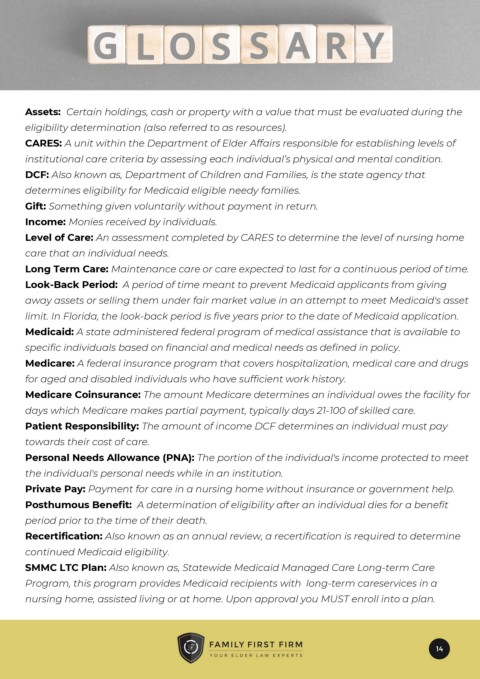
Assets: Certain holdings, cash or property with a value that must be evaluated during the
eligibility determination (also referred to as resources).
CARES: A unit within the Department of Elder Affairs responsible for establishing levels of
institutional care criteria by assessing each individual’s physical and mental condition.
DCF: Also known as, Department of Children and Families, is the state agency that
determines eligibility for Medicaid eligible needy families.
Gift: Something given voluntarily without payment in return.
Income: Monies received by individuals.
Level of Care: An assessment completed by CARES to determine the level of nursing home
care that an individual needs.
Long Term Care: Maintenance care or care expected to last for a continuous period of time.
Look-Back Period: A period of time meant to prevent Medicaid applicants from giving
away assets or selling them under fair market value in an attempt to meet Medicaid's asset
limit. In Florida, the look-back period is five years prior to the date of Medicaid application.
Medicaid: A state administered federal program of medical assistance that is available to
specific individuals based on financial and medical needs as defined in policy.
Medicare: A federal insurance program that covers hospitalization, medical care and drugs
for aged and disabled individuals who have sufficient work history.
Medicare Coinsurance: The amount Medicare determines an individual owes the facility for
days which Medicare makes partial payment, typically days 21-100 of skilled care.
Patient Responsibility: The amount of income DCF determines an individual must pay
towards their cost of care.
Personal Needs Allowance (PNA): The portion of the individual's income protected to meet
the individual's personal needs while in an institution.
Private Pay: Payment for care in a nursing home without insurance or government help.
Posthumous Benefit: A determination of eligibility after an individual dies for a benefit
period prior to the time of their death.
Recertification: Also known as an annual review, a recertification is required to determine
continued Medicaid eligibility.
SMMC LTC Plan: Also known as, Statewide Medicaid Managed Care Long-term Care
Program, this program provides Medicaid recipients with long-term careservices in a
nursing home, assisted living or at home. Upon approval you MUST enroll into a plan.
14