Page 42 - 2020 Barrister Employee Benefits Book
P. 42
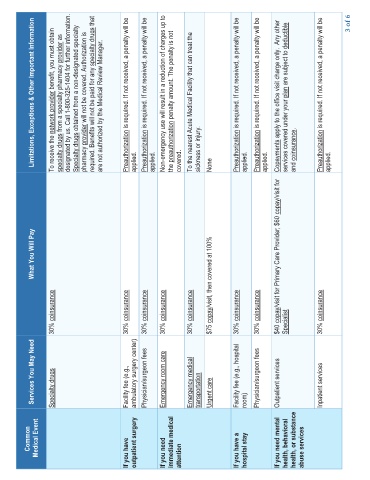
Limitations, Exceptions & Other Important Information
network provider benefit, you must obtain provider as designated by us. Call 1-800-325-1404 for further information. Specialty drugs obtained from a non-designated specialty provider will not be covered. Authorization is specialty drugs that are not authorized by the Medical Review Manager. Preauthorization is required. If not received, a penalty will be Preauthorization is required. If not received, a penalty will be Non-emergency use will result in a reduction
To receive the specialty drugs from a specialty pharmacy pharmacy required. Benefits will not be paid for any applied. applied. the covered. sickness or injury. None applied. applied. services covered under your coinsurance. and applied.
copay/visit for
What You Will Pay copay/visit for Primary Care Provider; $60
coinsurance coinsurance coinsurance coinsurance coinsurance copay/visit, then covered at 100% coinsurance coinsurance coinsurance
30% 30% 30% 30% 30% $75 30% 30% $40 Specialist 30%
Services You May Need Specialty drugs Facility fee (e.g., ambulatory surgery center) Physician/surgeon fees Emergency room care Emergency medical transportation Urgent care Facility fee (e.g., hospital room) Physician/surgeon fees Outpatient services Inpatient services
Common Medical Event If you have outpatient surgery If you need immediate medical attention If you have a hospital stay If you need mental health, behavioral health, or substance abuse services