Page 41 - WestCalcasieuCameron2017
P. 41
PREPARING FOR DISCHARGE
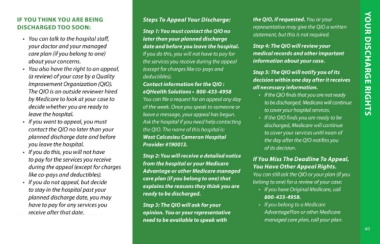
Most insurance companies have clause. At the time of service, you SELF-PAY PATIENTS IF YOU THINK YOU ARE BEING Steps To Appeal Your Discharge: the QIO, if requested. You or your
COB provisions that determine who will be asked to answer questions to The Patient Financial Services DISCHARGED TOO SOON: representative may give the QIO a written
is the primary payer when medical help determine the primary insurance Department will send statements for • You can talk to the hospital staff, Step 1: You must contact the QIO no statement, but this is not required.
expenses are incurred. This prevents carrier paying for your visit. This payment of self-pay accounts. You will your doctor and your managed later than your planned discharge Step 4: The QIO will review your
duplicate payments. COB priority must is referred to as an MSP (Medicare receive two to three billing statements care plan (if you belong to one) date and before you leave the hospital. medical records and other important
be identified at admission in order to Secondary Payer) Questionnaire and over a 90-day period to obtain a about your concerns. If you do this, you will not have to pay for information about your case.
comply with insurance guidelines. Your is required by federal law. Providing payment or to make payment arrange- • You also have the right to an appeal, the services you receive during the appeal YOUR DISCHARGE RIGHTS
insurance may request a completed accurate information will allow us to bill ments. If payment arrangements are (a review) of your case by a Quality (except for charges like co-pays and Step 5: The QIO will notify you of its
COB form before paying a claim and the correct insurance company. not established and no payment is Improvement Organization (QIO). deductibles). decision within one day after it receives
every attempt will be made to notify Medicare deductibles and co-insurance made during the 90-day period, the The QIO is an outside reviewer hired Contact information for the QIO : all necessary information.
you if this occurs. The hospital cannot are covered by your secondary account will be placed with a collection by Medicare to look at your case to eQHealth Solutions • 800-433-4958 • If the QIO finds that you are not ready
provide this information to your insurance. If you do not have secondary agency. If you need an itemized decide whether you are ready to You can file a request for an appeal any day to be discharged, Medicare will continue
insurance company. You must resolve insurance, you will be asked to pay statement of your account. leave the hospital. of the week. Once you speak to someone or to cover your hospital services.
this issue with your insurance carrier in these amounts or establish a payment If you have questions call the • If you want to appeal, you must leave a message, your appeal has begun. • If the QIO finds you are ready to be
order for the claim to be paid. plan. If you are unable to pay these Patient Financial Services Dept. contact the QIO no later than your Ask the hospital if you need help contacting discharged, Medicare will continue
amounts, we will help you determine if at 337-527-4232. the QIO. The name of this hospital is: to cover your services until noon of
MEDICAID you qualify for a state funded program. planned discharge date and before West Calcasieu Cameron Hospital the day after the QIO notifies you
We will need a copy of your Medicaid you leave the hospital. Provider #190013. of its decision.
card for the current month. Medicaid COMMERCIAL INSURANCE UNINSURED PATIENTS • If you do this, you will not have
has payment limitations on a number As a service to our customers, we will A representative from Admissions to pay for the services you receive Step 2: You will receive a detailed notice If You Miss The Deadline To Appeal,
of services and items. Medicaid does forward a claim to your commercial or Patient Financial Services will during the appeal (except for charges from the hospital or your Medicare You Have Other Appeal Rights.
not pay for the cost of a private room insurance carrier based on the discuss financial arrangements with like co-pays and deductibles). Advantage or other Medicare managed You can still ask the QIO or your plan (if you
unless medically necessary. information you provide at the time of you. A hospital representative is • If you do not appeal, but decide care plan (if you belong to one) that belong to one) for a review of your case:
registration. Please provide all related available to assist you in applying for to stay in the hospital past your explains the reasons they think you are • If you have Original Medicare, call
MEDICARE information such as policy number, Medicaid, charity application or other planned discharge date, you may ready to be discharged. 800-433-4958.
This hospital is an approved Medicare group number and the correct mailing government assistance programs. have to pay for any services you • If you belong to a Medicare
provider. All services billed to address for your insurance company. receive after that date. Step 3: The QIO will ask for your AdvantagePlan or other Medicare
Medicare follow federal guidelines opinion. You or your representative managed care plan, call your plan.
and procedures. Medicare has a COB need to be available to speak with
39 40