Page 485 - Fluid, Electrolyte, and Acid-Base Disorders in Small Animal Practice
P. 485
Fluid, Electrolyte, and Acid-Base Disturbances in Liver Disease 473
arteriolar tone to regulate the GFR and filtration fraction. cirrhosis and ascites. 147 A similar syndrome rarely may
Redistribution of blood flow from the outer cortical to occur in veterinary patients. Reduced renal cortical perfu-
juxtamedullary nephrons occurs in approximately 60% sion resulting from increased renal vascular resistance
of human patients with ascites. Redistribution of renal precedes renal failure in this syndrome. The cause of
blood flow and increased intrarenal arterial resistance intrarenal vasoconstriction is complex and poorly under-
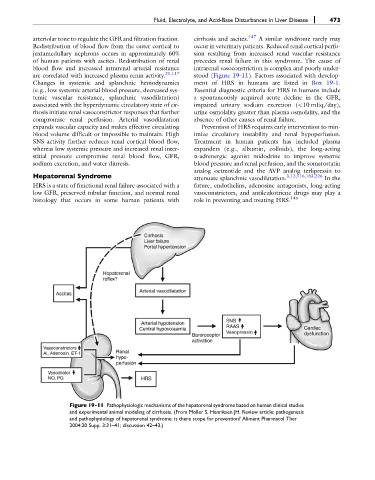
are correlated with increased plasma renin activity. 21,117 stood (Figure 19-11). Factors associated with develop-
Changes in systemic and splanchnic hemodynamics ment of HRS in humans are listed in Box 19-1.
(e.g., low systemic arterial blood pressure, decreased sys- Essential diagnostic criteria for HRS in humans include
temic vascular resistance, splanchnic vasodilatation) a spontaneously acquired acute decline in the GFR,
associated with the hyperdynamic circulatory state of cir- impaired urinary sodium excretion (<10 mEq/day),
rhosis initiate renal vasoconstrictor responses that further urine osmolality greater than plasma osmolality, and the
compromise renal perfusion. Arterial vasodilatation absence of other causes of renal failure.
expands vascular capacity and makes effective circulating Prevention of HRS requires early intervention to min-
blood volume difficult or impossible to maintain. High imize circulatory instability and renal hypoperfusion.
SNS activity further reduces renal cortical blood flow, Treatment in human patients has included plasma
whereas low systemic pressure and increased renal inter- expanders (e.g., albumin, colloids), the long-acting
stitial pressure compromise renal blood flow, GFR, a-adrenergic agonist midodrine to improve systemic
sodium excretion, and water diuresis. blood pressure and renal perfusion, and the somatostatin
analog octreotide and the AVP analog terlipressin to
Hepatorenal Syndrome attenuate splanchnic vasodilatation. 3,12,116,183,226 In the
HRS is a state of functional renal failure associated with a future, endothelins, adenosine antagonists, long-acting
low GFR, preserved tubular function, and normal renal vasoconstrictors, and antileukotriene drugs may play a
histology that occurs in some human patients with role in preventing and treating HRS. 146
Figure 19-11 Pathophysiologic mechanisms of the hepatorenal syndrome based on human clinical studies
and experimental animal modeling of cirrhosis. (From Moller S, Henriksen JH. Review article: pathogenesis
and pathophysiology of hepatorenal syndrome: is there scope for prevention? Aliment Pharmacol Ther
2004;20 Supp. 3:31–41; discussion 42–43.)