Page 524 - Small Animal Internal Medicine, 6th Edition
P. 524
496 PART III Digestive System Disorders
hyperechoic intestinal mucosal striations at ultrasound is However, a few dilated lacteals may be found in any normal
very suggestive of lymphangiectasia (Fig. 31.8), but the sen- dog. Not seeing mucosal striations at ultrasonography or
VetBooks.ir sitivity of this finding for lymphangiectasia is uncertain. dilated lacteals at endoscopy does not lessen the chance of
lymphangiectasia because the disease may be confined to a
Diagnosis generally requires intestinal histopathology, but
gross endoscopic appearance can sometimes be diagnostic.
When biopsying, high-quality tissue samples are critical.
It is important to perform ileoscopy as well as duodenoscopy. section of bowel not examined by ultrasound or endoscopy.
Feeding fat the night before endoscopy or ultrasonography Submitting distorted, poorly oriented mucosal fragments
seems to make diagnosis easier. If numerous dilated lacteals or shredded villi makes it difficult to diagnose lymphangi-
(Fig. 31.9) are seen endoscopically in a patient that is hypoal- ectasia. Surgical biopsies are sometimes required. Finding
buminemic due to PLE, one may diagnose lymphangiectasia. lipogranulomas (Fig. 31.10) or obviously dilated, tortuous
lymphatics on the intestines during surgery is extremely sug-
gestive of IL.
Treatment
The underlying cause of IL is rarely determined, necessitat-
ing reliance on symptomatic therapy. An ultra–low-fat diet
essentially devoid of long-chain fatty acids helps prevent
further intestinal lacteal engorgement and subsequent
protein loss. In many cases diagnosed early, this dietary
therapy alone will cause the serum albumin to undergo a
major increase within 7 to 12 days. More advanced cases
will require concurrent prednisolone (1.1-2.2 mg/kg/day
PO) or cyclosporine (3-5 mg/kg PO q12h) therapy. Cases
that respond to diet alone may ultimately benefit from a
2- to 3-month course of prednisolone or cyclosporine to
help prevent enlargement of lipogranulomas with sub-
sequent relapse. If cyclosporine is used and the patient is
not responding, therapeutic drug monitoring is indicated.
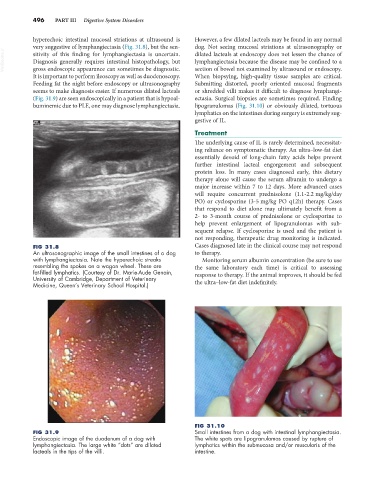
FIG 31.8 Cases diagnosed late in the clinical course may not respond
An ultrasonographic image of the small intestines of a dog to therapy.
with lymphangiectasia. Note the hyperechoic streaks Monitoring serum albumin concentration (be sure to use
resembling the spokes on a wagon wheel. These are the same laboratory each time) is critical to assessing
fat-filled lymphatics. (Courtesy of Dr. Marie-Aude Genain, response to therapy. If the animal improves, it should be fed
University of Cambridge, Department of Veterinary
Medicine, Queen’s Veterinary School Hospital.) the ultra–low-fat diet indefinitely.
FIG 31.10
FIG 31.9 Small intestines from a dog with intestinal lymphangiectasia.
Endoscopic image of the duodenum of a dog with The white spots are lipogranulomas caused by rupture of
lymphangiectasia. The large white “dots” are dilated lymphatics within the submucosa and/or muscularis of the
lacteals in the tips of the villi. intestine.