Page 304 - Clinical Small Animal Internal Medicine
P. 304
272 Section 3 Cardiovascular Disease
VetBooks.ir Cat with suspected subclinical myocardial disease
Auscultation
ECG Arrhythmia Gallop Murmur
T4 (if >7 years) BP PCV
Tachyarrhythmia BP, PCV (T4) normal PCV low Consider anemia
“In-house” Echo Systemic BP high Consider hypertension
disease
Normal LA, or
Obvious LA echo not available T4 high Consider hyperthyroidism
enlargement
Additional tests
NT-proBNP Thoracic
radiography
High NT-proBNP
No cardiomegaly
“High-risk” Cardiomegaly Low NT-proBNP
heart disease Normal or “Low-risk”
e
e
heart disease
Referral echo?
Annual re-test
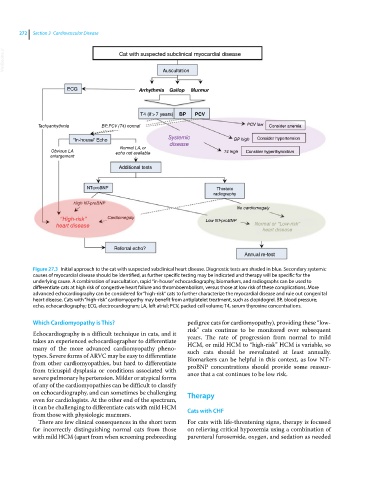
Figure 27.3 Initial approach to the cat with suspected subclinical heart disease. Diagnostic tests are shaded in blue. Secondary systemic
causes of myocardial disease should be identified, as further specific testing may be indicated and therapy will be specific for the
underlying cause. A combination of auscultation, rapid “in‐house” echocardiography, biomarkers, and radiographs can be used to
differentiate cats at high risk of congestive heart failure and thromboembolism, versus those at low risk of these complications. More
advanced echocardiography can be considered for “high‐risk” cats to further characterize the myocardial disease and rule out congenital
heart disease. Cats with “high‐risk” cardiomyopathy may benefit from antiplatelet treatment, such as clopidogrel. BP, blood pressure;
echo, echocardiography; ECG, electrocardiogram; LA, left atrial; PCV, packed cell volume; T4, serum thyroxine concentrations.
Which Cardiomyopathy is This? pedigree cats for cardiomyopathy), providing these “low‐
risk” cats continue to be monitored over subsequent
Echocardiography is a difficult technique in cats, and it years. The rate of progression from normal to mild
takes an experienced echocardiographer to differentiate HCM, or mild HCM to “high‐risk” HCM is variable, so
many of the more advanced cardiomyopathy pheno- such cats should be reevaluated at least annually.
types. Severe forms of ARVC may be easy to differentiate Biomarkers can be helpful in this context, as low NT‐
from other cardiomyopathies, but hard to differentiate proBNP concentrations should provide some reassur-
from tricuspid dysplasia or conditions associated with ance that a cat continues to be low risk.
severe pulmonary hypertension. Milder or atypical forms
of any of the cardiomyopathies can be difficult to classify
on echocardiography, and can sometimes be challenging Therapy
even for cardiologists. At the other end of the spectrum,
it can be challenging to differentiate cats with mild HCM Cats with CHF
from those with physiologic murmurs.
There are few clinical consequences in the short term For cats with life‐threatening signs, therapy is focused
for incorrectly distinguishing normal cats from those on relieving critical hypoxemia using a combination of
with mild HCM (apart from when screening prebreeding parenteral furosemide, oxygen, and sedation as needed