Page 8 - SBCEO Benefit Guide 19-20_FINAL
P. 8
Medical Benefits 8
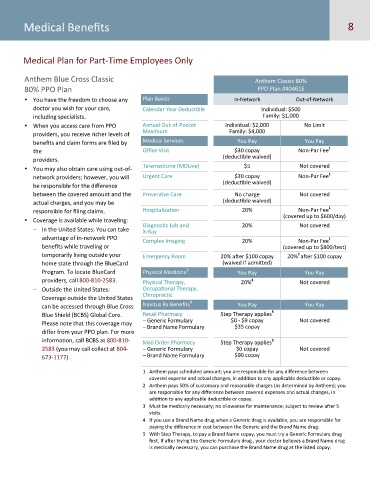
Medical Plan for Part-Time Employees Only
Anthem Blue Cross Classic Anthem Classic 80%
80% PPO Plan PPO Plan #40461E
You have the freedom to choose any Plan Basics In-Network Out-of-Network
doctor you wish for your care, Calendar Year Deductible Individual: $500
including specialists. Family: $1,000
When you access care from PPO Annual Out-of-Pocket Individual: $2,000 No Limit
Maximum Family: $4,000
providers, you receive richer levels of
benefits and claim forms are filed by Medical Services You Pay You Pay
1
the Office Visit $30 copay Non-Par Fee
(deductible waived)
providers.
Telemedicine (MDLive) $5 Not covered
You may also obtain care using out-of-
1
network providers; however, you will Urgent Care $30 copay Non-Par Fee
(deductible waived)
be responsible for the difference
between the covered amount and the Preventive Care No charge Not covered
actual charges, and you may be (deductible waived)
1
responsible for filing claims. Hospitalization 20% Non-Par Fee
(covered up to $600/day)
Coverage is available while traveling:
Diagnostic Lab and 20% Not covered
− In the United States: You can take X-Ray
advantage of in-network PPO 1
Complex Imaging 20% Non-Par Fee
benefits while traveling or (covered up to $800/test)
2
temporarily living outside your Emergency Room 20% after $100 copay 20% after $100 copay
home state through the BlueCard (waived if admitted)
3
Program. To locate BlueCard Physical Medicine You Pay You Pay
providers, call 800-810-2583. Physical Therapy, 20% Not covered
3
− Outside the United States: Occupational Therapy,
Chiropractic
Coverage outside the United States 4
can be accessed through Blue Cross Navitus Rx Benefits You Pay You Pay
5
Blue Shield (BCBS) Global Core. Retail Pharmacy Step Therapy applies
− Generic Formulary $0 - $9 copay Not covered
Please note that this coverage may
− Brand Name Formulary $35 copay
differ from your PPO plan. For more
information, call BCBS at 800-810- Mail Order Pharmacy Step Therapy applies
5
2583 (you may call collect at 804- − Generic Formulary $0 copay Not covered
673-1177) . − Brand Name Formulary $90 copay
1 Anthem pays scheduled amount; you are responsible for any difference between
covered expense and actual changes, in addition to any applicable deductible or copay.
2 Anthem pays 50% of customary and reasonable charges (as determined by Anthem); you
are responsible for any difference between covered expenses and actual changes, in
addition to any applicable deductible or copay.
3 Must be medically necessary; no allowance for maintenance; subject to review after 5
visits.
4 If you use a Brand Name drug when a Generic drug is available, you are responsible for
paying the difference in cost between the Generic and the Brand Name drug.
5 With Step Therapy, to pay a Brand Name copay, you must try a Generic Formulary drug
first. If after trying the Generic Formulary drug , your doctor believes a Brand Name drug
is medically necessary, you can purchase the Brand Name drug at the listed copay.