Page 7 - Wayfinders EE Guide 03-18
P. 7
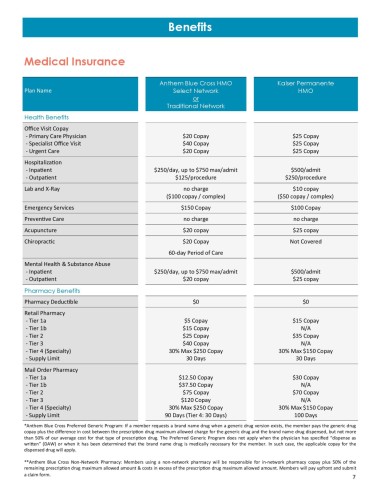
Benefits
Medical Insurance
Anthem Blue Cross HMO Kaiser Permanente
Plan Name Select Network HMO
or
Traditional Network
Health Benefits
Office Visit Copay
- Primary Care Physician $20 Copay $25 Copay
- Specialist Office Visit $40 Copay $25 Copay
- Urgent Care $20 Copay $25 Copay
Hospitalization
- Inpatient $250/day, up to $750 max/admit $500/admit
- Outpatient $125/procedure $250/procedure
Lab and X-Ray no charge $10 copay
($100 copay / complex) ($50 copay / complex)
Emergency Services $150 Copay $100 Copay
Preventive Care no charge no charge
Acupuncture $20 copay $25 copay
Chiropractic $20 Copay Not Covered
60-day Period of Care
Mental Health & Substance Abuse
- Inpatient $250/day, up to $750 max/admit $500/admit
- Outpatient $20 copay $25 copay
Pharmacy Benefits
Pharmacy Deductible $0 $0
Retail Pharmacy
- Tier 1a $5 Copay $15 Copay
- Tier 1b $15 Copay N/A
- Tier 2 $25 Copay $35 Copay
- Tier 3 $40 Copay N/A
- Tier 4 (Specialty) 30% Max $250 Copay 30% Max $150 Copay
- Supply Limit 30 Days 30 Days
Mail Order Pharmacy
- Tier 1a $12.50 Copay $30 Copay
- Tier 1b $37.50 Copay N/A
- Tier 2 $75 Copay $70 Copay
- Tier 3 $120 Copay N/A
- Tier 4 (Specialty) 30% Max $250 Copay 30% Max $150 Copay
- Supply Limit 90 Days (Tier 4: 30 Days) 100 Days
*Anthem Blue Cross Preferred Generic Program: If a member requests a brand name drug when a generic drug version exists, the member pays the generic drug
copay plus the difference in cost between the prescription drug maximum allowed charge for the generic drug and the brand name drug dispensed, but not more
than 50% of our average cost for that type of prescription drug. The Preferred Generic Program does not apply when the physician has specified “dispense as
written” (DAW) or when it has been determined that the brand name drug is medically necessary for the member. In such case, the applicable copay for the
dispensed drug will apply.
**Anthem Blue Cross Non-Network Pharmacy: Members using a non-network pharmacy will be responsible for in-network pharmacy copay plus 50% of the
remaining prescription drug maximum allowed amount & costs in excess of the prescription drug maximum allowed amount. Members will pay upfront and submit
a claim form.
7