Page 11 - 2022 Penn Engineering Guide
P. 11
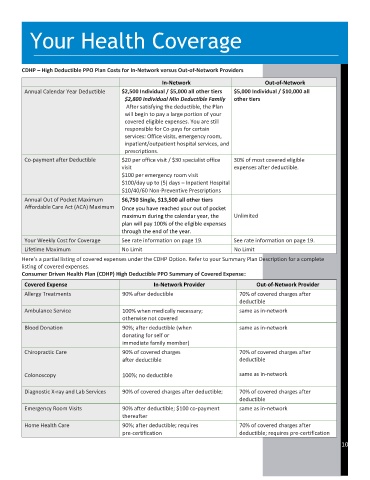
Your Health Coverage
CDHP – High Deductible PPO Plan Costs for In-Network versus Out-of-Network Providers
In-Network Out-of-Network
Annual Calendar Year Deductible $2,500 Individual / $5,000 all other tiers $5,000 Individual / $10,000 all
$2,800 Individual Min Deductible Family other tiers
After satisfying the deductible, the Plan
will begin to pay a large portion of your
covered eligible expenses. You are still
responsible for Co-pays for certain
services: Office visits, emergency room,
inpatient/outpatient hospital services, and
prescriptions.
Co-payment after Deductible $20 per office visit / $30 specialist office 30% of most covered eligible
visit expenses after deductible.
$100 per emergency room visit
$100/day up to (5) days – Inpatient Hospital
$10/40/60 Non-Preventive Prescriptions
Annual Out of Pocket Maximum $6,750 Single, $13,500 all other tiers
Affordable Care Act (ACA) Maximum Once you have reached your out of pocket
maximum during the calendar year, the Unlimited
plan will pay 100% of the eligible expenses
through the end of the year.
Your Weekly Cost for Coverage See rate information on page 19. See rate information on page 19.
Lifetime Maximum No Limit No Limit
Here’s a partial listing of covered expenses under the CDHP Option. Refer to your Summary Plan Description for a complete
listing of covered expenses.
Consumer Driven Health Plan (CDHP) High Deductible PPO Summary of Covered Expense:
Covered Expense In-Network Provider Out-of-Network Provider
Allergy Treatments 90% after deductible 70% of covered charges after
deductible
Ambulance Service 100% when medically necessary; same as in-network
otherwise not covered
Blood Donation 90%; after deductible (when same as in-network
donating for self or
immediate family member)
Chiropractic Care 90% of covered charges 70% of covered charges after
after deductible deductible
Colonoscopy 100%; no deductible same as in-network
Diagnostic X-ray and Lab Services 90% of covered charges after deductible; 70% of covered charges after
deductible
Emergency Room Visits 90% after deductible; $100 co-payment same as in-network
thereafter
Home Health Care 90%; after deductible; requires 70% of covered charges after
pre-certification deductible; requires pre-certification
10