Page 6 - Leona Arizona Employment Group Flipbook
P. 6
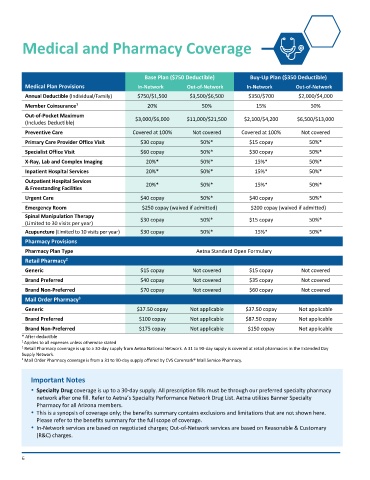
Medical and Pharmacy Coverage
Base Plan ($750 Deductible) Buy-Up Plan ($350 Deductible)
Medical Plan Provisions In-Network Out-of-Network In-Network Out-of-Network
Annual Deductible (Individual/Family) $750/$1,500 $3,500/$6,500 $350/$700 $2,000/$4,000
1
Member Coinsurance 20% 50% 15% 50%
Out-of-Pocket Maximum $3,000/$6,000 $11,000/$21,500 $2,100/$4,200 $6,500/$13,000
(Includes Deductible)
Preventive Care Covered at 100% Not covered Covered at 100% Not covered
Primary Care Provider Office Visit $30 copay 50%* $15 copay 50%*
Specialist Office Visit $60 copay 50%* $30 copay 50%*
X-Ray, Lab and Complex Imaging 20%* 50%* 15%* 50%*
Inpatient Hospital Services 20%* 50%* 15%* 50%*
Outpatient Hospital Services
& Freestanding Facilities 20%* 50%* 15%* 50%*
Urgent Care $40 copay 50%* $40 copay 50%*
Emergency Room $250 copay (waived if admitted) $200 copay (waived if admitted)
Spinal Manipulation Therapy $30 copay 50%* $15 copay 50%*
(Limited to 30 visits per year)
Acupuncture (Limited to 10 visits per year) $30 copay 50%* 15%* 50%*
Pharmacy Provisions
Pharmacy Plan Type Aetna Standard Open Formulary
2
Retail Pharmacy
Generic $15 copay Not covered $15 copay Not covered
Brand Preferred $40 copay Not covered $35 copay Not covered
Brand Non-Preferred $70 copay Not covered $60 copay Not covered
3
Mail Order Pharmacy
Generic $37.50 copay Not applicable $37.50 copay Not applicable
Brand Preferred $100 copay Not applicable $87.50 copay Not applicable
Brand Non-Preferred $175 copay Not applicable $150 copay Not applicable
* After deductible
1 Applies to all expenses unless otherwise stated
2 Retail Pharmacy coverage is up to a 30-day supply from Aetna National Network. A 31 to 90-day supply is covered at retail pharmacies in the Extended Day
Supply Network.
3 Mail Order Pharmacy coverage is from a 31 to 90-day supply offered by CVS Caremark® Mail Service Pharmacy.
Important Notes
Specialty Drug coverage is up to a 30-day supply. All prescription fills must be through our preferred specialty pharmacy
network after one fill. Refer to Aetna’s Specialty Performance Network Drug List. Aetna utilizes Banner Specialty
Pharmacy for all Arizona members.
This is a synopsis of coverage only; the benefits summary contains exclusions and limitations that are not shown here.
Please refer to the benefits summary for the full scope of coverage.
In-Network services are based on negotiated charges; Out-of-Network services are based on Reasonable & Customary
(R&C) charges.
6