Page 21 - Tessenderlo Kerley, Inc 2022 Benefit Guide
P. 21
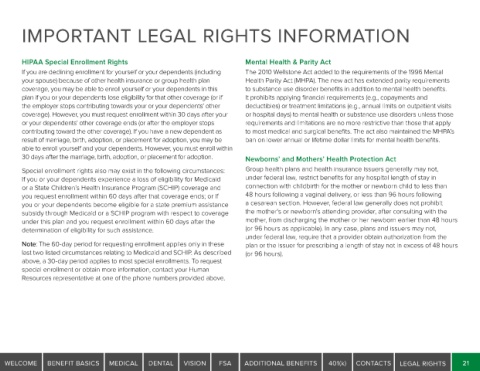
IMPORTANT LEGAL RIGHTS INFORMATION
HIPAA Special Enrollment Rights Mental Health & Parity Act
If you are declining enrollment for yourself or your dependents (including The 2010 Wellstone Act added to the requirements of the 1996 Mental
your spouse) because of other health insurance or group health plan Health Parity Act (MHPA). The new act has extended parity requirements
coverage, you may be able to enroll yourself or your dependents in this to substance use disorder benefits in addition to mental health benefits.
plan if you or your dependents lose eligibility for that other coverage (or if It prohibits applying financial requirements (e.g., copayments and
the employer stops contributing towards your or your dependents’ other deductibles) or treatment limitations (e.g., annual limits on outpatient visits
coverage). However, you must request enrollment within 30 days after your or hospital days) to mental health or substance use disorders unless those
or your dependents’ other coverage ends (or after the employer stops requirements and limitations are no more restrictive than those that apply
contributing toward the other coverage). If you have a new dependent as to most medical and surgical benefits. The act also maintained the MHPA’s
result of marriage, birth, adoption, or placement for adoption, you may be ban on lower annual or lifetime dollar limits for mental health benefits.
able to enroll yourself and your dependents. However, you must enroll within
30 days after the marriage, birth, adoption, or placement for adoption. Newborns’ and Mothers’ Health Protection Act
Special enrollment rights also may exist in the following circumstances: Group health plans and health insurance issuers generally may not,
If you or your dependents experience a loss of eligibility for Medicaid under federal law, restrict benefits for any hospital length of stay in
or a State Children’s Health Insurance Program (SCHIP) coverage and connection with childbirth for the mother or newborn child to less than
you request enrollment within 60 days after that coverage ends; or If 48 hours following a vaginal delivery, or less than 96 hours following
you or your dependents become eligible for a state premium assistance a cesarean section. However, federal law generally does not prohibit
subsidy through Medicaid or a SCHIP program with respect to coverage the mother's or newborn's attending provider, after consulting with the
under this plan and you request enrollment within 60 days after the mother, from discharging the mother or her newborn earlier than 48 hours
determination of eligibility for such assistance. (or 96 hours as applicable). In any case, plans and issuers may not,
under federal law, require that a provider obtain authorization from the
Note: The 60-day period for requesting enrollment applies only in these plan or the issuer for prescribing a length of stay not in excess of 48 hours
last two listed circumstances relating to Medicaid and SCHIP. As described (or 96 hours).
above, a 30-day period applies to most special enrollments. To request
special enrollment or obtain more information, contact your Human
Resources representative at one of the phone numbers provided above.
WELCOME BENEFIT BASICS MEDICAL DENTAL VISION FSA ADDITIONAL BENEFITS 401(k) CONTACTS LEGAL RIGHTS 21