Page 14 - Gastrointestinal Bleeding (Xuất huyết tiêu hóa)
P. 14
288 PART III Symptoms, Signs, and Biopsychosocial Issues
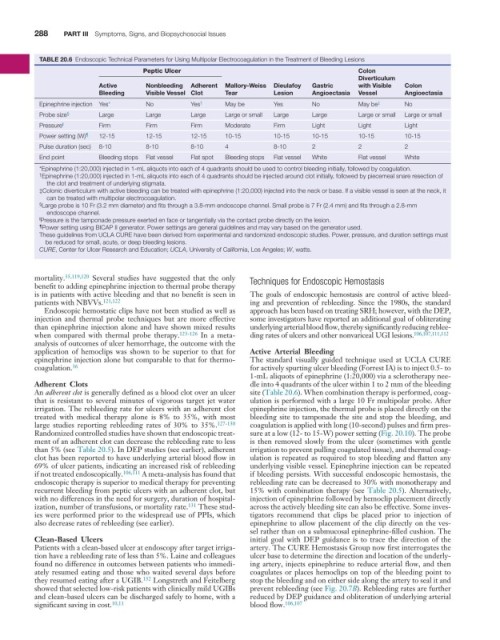
TABLE 20.6 Endoscopic Technical Parameters for Using Multipolar Electrocoagulation in the Treatment of Bleeding Lesions
Peptic Ulcer Colon
Diverticulum
Active Nonbleeding Adherent Mallory-Weiss Dieulafoy Gastric with Visible Colon
Bleeding Visible Vessel Clot Tear Lesion Angioectasia Vessel Angioectasia
Epinephrine injection Yes* No Yes † May be Yes No May be ‡ No
Probe size § Large Large Large Large or small Large Large Large or small Large or small
Pressure ∥ Firm Firm Firm Moderate Firm Light Light Light
Power setting (W) ¶ 12-15 12-15 12-15 10-15 10-15 10-15 10-15 10-15
Pulse duration (sec) 8-10 8-10 8-10 4 8-10 2 2 2
End point Bleeding stops Flat vessel Flat spot Bleeding stops Flat vessel White Flat vessel White
*Epinephrine (1:20,000) injected in 1-mL aliquots into each of 4 quadrants should be used to control bleeding initially, followed by coagulation.
† Epinephrine (1:20,000) injected in 1-mL aliquots into each of 4 quadrants should be injected around clot initially, followed by piecemeal snare resection of
the clot and treatment of underlying stigmata.
‡Colonic diverticulum with active bleeding can be treated with epinephrine (1:20,000) injected into the neck or base. If a visible vessel is seen at the neck, it
can be treated with multipolar electrocoagulation.
§ Large probe is 10 Fr (3.2 mm diameter) and fits through a 3.8-mm endoscope channel. Small probe is 7 Fr (2.4 mm) and fits through a 2.8-mm
endoscope channel.
∥ Pressure is the tamponade pressure exerted en face or tangentially via the contact probe directly on the lesion.
¶ Power setting using BICAP II generator. Power settings are general guidelines and may vary based on the generator used.
These guidelines from UCLA CURE have been derived from experimental and randomized endoscopic studies. Power, pressure, and duration settings must
be reduced for small, acute, or deep bleeding lesions.
CURE, Center for Ulcer Research and Education; UCLA, University of California, Los Angeles; W, watts.
mortality. 35,119,120 Several studies have suggested that the only Techniques for Endoscopic Hemostasis
benefit to adding epinephrine injection to thermal probe therapy
is in patients with active bleeding and that no benefit is seen in The goals of endoscopic hemostasis are control of active bleed-
patients with NBVVs. 121,122 ing and prevention of rebleeding. Since the 1980s, the standard
Endoscopic hemostatic clips have not been studied as well as approach has been based on treating SRH; however, with the DEP,
injection and thermal probe techniques but are more effective some investigators have reported an additional goal of obliterating
than epinephrine injection alone and have shown mixed results underlying arterial blood flow, thereby significantly reducing reblee-
when compared with thermal probe therapy. 123-126 In a meta- ding rates of ulcers and other nonvariceal UGI lesions. 106,107,111,112
analysis of outcomes of ulcer hemorrhage, the outcome with the
application of hemoclips was shown to be superior to that for Active Arterial Bleeding
epinephrine injection alone but comparable to that for thermo- The standard visually guided technique used at UCLA CURE
36
coagulation. for actively spurting ulcer bleeding (Forrest IA) is to inject 0.5- to
1-mL aliquots of epinephrine (1:20,000) via a sclerotherapy nee-
Adherent Clots dle into 4 quadrants of the ulcer within 1 to 2 mm of the bleeding
An adherent clot is generally defined as a blood clot over an ulcer site (Table 20.6). When combination therapy is performed, coag-
that is resistant to several minutes of vigorous target jet water ulation is performed with a large 10 Fr multipolar probe. After
irrigation. The rebleeding rate for ulcers with an adherent clot epinephrine injection, the thermal probe is placed directly on the
treated with medical therapy alone is 8% to 35%, with most bleeding site to tamponade the site and stop the bleeding, and
large studies reporting rebleeding rates of 30% to 35%. 127-130 coagulation is applied with long (10-second) pulses and firm pres-
Randomized controlled studies have shown that endoscopic treat- sure at a low (12- to 15-W) power setting (Fig. 20.10). The probe
ment of an adherent clot can decrease the rebleeding rate to less is then removed slowly from the ulcer (sometimes with gentle
than 5% (see Table 20.5). In DEP studies (see earlier), adherent irrigation to prevent pulling coagulated tissue), and thermal coag-
clot has been reported to have underlying arterial blood flow in ulation is repeated as required to stop bleeding and flatten any
69% of ulcer patients, indicating an increased risk of rebleeding underlying visible vessel. Epinephrine injection can be repeated
if not treated endoscopically. 106,111 A meta-analysis has found that if bleeding persists. With successful endoscopic hemostasis, the
endoscopic therapy is superior to medical therapy for preventing rebleeding rate can be decreased to 30% with monotherapy and
recurrent bleeding from peptic ulcers with an adherent clot, but 15% with combination therapy (see Table 20.5). Alternatively,
with no differences in the need for surgery, duration of hospital- injection of epinephrine followed by hemoclip placement directly
ization, number of transfusions, or mortality rate. 131 These stud- across the actively bleeding site can also be effective. Some inves-
ies were performed prior to the widespread use of PPIs, which tigators recommend that clips be placed prior to injection of
also decrease rates of rebleeding (see earlier). epinephrine to allow placement of the clip directly on the ves-
sel rather than on a submucosal epinephrine-filled cushion. The
Clean-Based Ulcers initial goal with DEP guidance is to trace the direction of the
Patients with a clean-based ulcer at endoscopy after target irriga- artery. The CURE Hemostasis Group now first interrogates the
tion have a rebleeding rate of less than 5%. Laine and colleagues ulcer base to determine the direction and location of the underly-
found no difference in outcomes between patients who immedi- ing artery, injects epinephrine to reduce arterial flow, and then
ately resumed eating and those who waited several days before coagulates or places hemoclips on top of the bleeding point to
they resumed eating after a UGIB. 132 Longstreth and Feitelberg stop the bleeding and on either side along the artery to seal it and
showed that selected low-risk patients with clinically mild UGIBs prevent rebleeding (see Fig. 20.7B). Rebleeding rates are further
and clean-based ulcers can be discharged safely to home, with a reduced by DEP guidance and obliteration of underlying arterial
significant saving in cost. 10,11 blood flow. 106,107