Page 15 - Gastrointestinal Bleeding (Xuất huyết tiêu hóa)
P. 15
CHAPTER 20 Gastrointestinal Bleeding 289
20
A B C
D E F
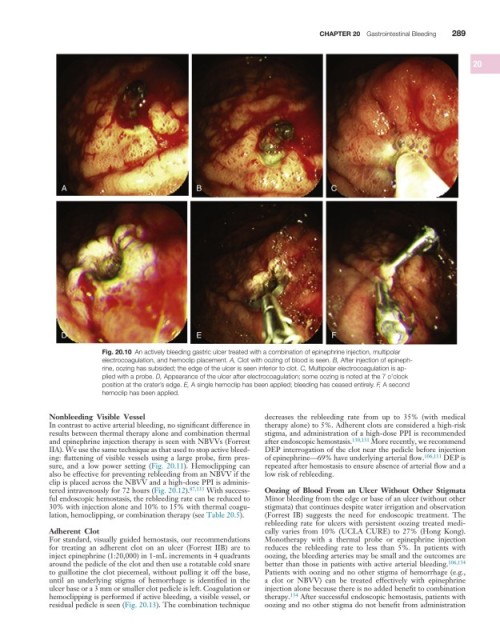
Fig. 20.10 An actively bleeding gastric ulcer treated with a combination of epinephrine injection, multipolar
electrocoagulation, and hemoclip placement. A, Clot with oozing of blood is seen. B, After injection of epineph-
rine, oozing has subsided; the edge of the ulcer is seen inferior to clot. C, Multipolar electrocoagulation is ap-
plied with a probe. D, Appearance of the ulcer after electrocoagulation; some oozing is noted at the 7 o’clock
position at the crater’s edge. E, A single hemoclip has been applied; bleeding has ceased entirely. F, A second
hemoclip has been applied.
Nonbleeding Visible Vessel decreases the rebleeding rate from up to 35% (with medical
In contrast to active arterial bleeding, no significant difference in therapy alone) to 5%. Adherent clots are considered a high-risk
results between thermal therapy alone and combination thermal stigma, and administration of a high-dose PPI is recommended
and epinephrine injection therapy is seen with NBVVs (Forrest after endoscopic hemostasis. 130,131 More recently, we recommend
IIA). We use the same technique as that used to stop active bleed- DEP interrogation of the clot near the pedicle before injection
ing: flattening of visible vessels using a large probe, firm pres- of epinephrine—69% have underlying arterial flow. 106,111 DEP is
sure, and a low power setting (Fig. 20.11). Hemoclipping can repeated after hemostasis to ensure absence of arterial flow and a
also be effective for preventing rebleeding from an NBVV if the low risk of rebleeding.
clip is placed across the NBVV and a high-dose PPI is adminis-
tered intravenously for 72 hours (Fig. 20.12). 87,133 With success- Oozing of Blood From an Ulcer Without Other Stigmata
ful endoscopic hemostasis, the rebleeding rate can be reduced to Minor bleeding from the edge or base of an ulcer (without other
30% with injection alone and 10% to 15% with thermal coagu- stigmata) that continues despite water irrigation and observation
lation, hemoclipping, or combination therapy (see Table 20.5). (Forrest IB) suggests the need for endoscopic treatment. The
rebleeding rate for ulcers with persistent oozing treated medi-
Adherent Clot cally varies from 10% (UCLA CURE) to 27% (Hong Kong).
For standard, visually guided hemostasis, our recommendations Monotherapy with a thermal probe or epinephrine injection
for treating an adherent clot on an ulcer (Forrest IIB) are to reduces the rebleeding rate to less than 5%. In patients with
inject epinephrine (1:20,000) in 1-mL increments in 4 quadrants oozing, the bleeding arteries may be small and the outcomes are
around the pedicle of the clot and then use a rotatable cold snare better than those in patients with active arterial bleeding. 106,134
to guillotine the clot piecemeal, without pulling it off the base, Patients with oozing and no other stigma of hemorrhage (e.g.,
until an underlying stigma of hemorrhage is identified in the a clot or NBVV) can be treated effectively with epinephrine
ulcer base or a 3 mm or smaller clot pedicle is left. Coagulation or injection alone because there is no added benefit to combination
hemoclipping is performed if active bleeding, a visible vessel, or therapy. 134 After successful endoscopic hemostasis, patients with
residual pedicle is seen (Fig. 20.13). The combination technique oozing and no other stigma do not benefit from administration