Page 4 - Gastrointestinal Bleeding (Xuất huyết tiêu hóa)
P. 4
278 PART III Symptoms, Signs, and Biopsychosocial Issues
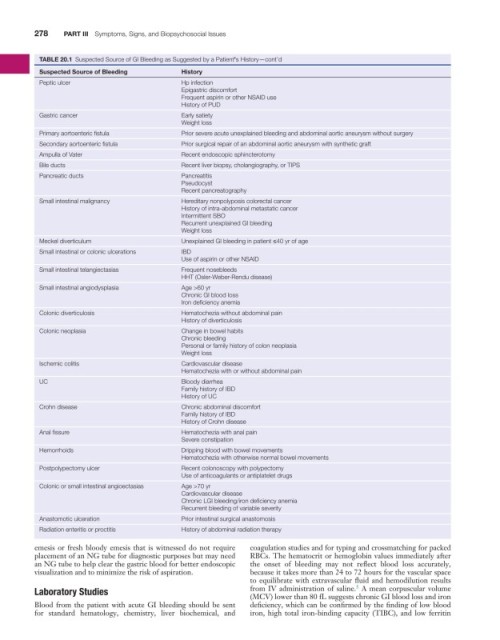
TABLE 20.1 Suspected Source of GI Bleeding as Suggested by a Patient’s History—cont’d
Suspected Source of Bleeding History
Peptic ulcer Hp infection
Epigastric discomfort
Frequent aspirin or other NSAID use
History of PUD
Gastric cancer Early satiety
Weight loss
Primary aortoenteric fistula Prior severe acute unexplained bleeding and abdominal aortic aneurysm without surgery
Secondary aortoenteric fistula Prior surgical repair of an abdominal aortic aneurysm with synthetic graft
Ampulla of Vater Recent endoscopic sphincterotomy
Bile ducts Recent liver biopsy, cholangiography, or TIPS
Pancreatic ducts Pancreatitis
Pseudocyst
Recent pancreatography
Small intestinal malignancy Hereditary nonpolyposis colorectal cancer
History of intra-abdominal metastatic cancer
Intermittent SBO
Recurrent unexplained GI bleeding
Weight loss
Meckel diverticulum Unexplained GI bleeding in patient ≤40 yr of age
Small intestinal or colonic ulcerations IBD
Use of aspirin or other NSAID
Small intestinal telangiectasias Frequent nosebleeds
HHT (Osler-Weber-Rendu disease)
Small intestinal angiodysplasia Age >60 yr
Chronic GI blood loss
Iron deficiency anemia
Colonic diverticulosis Hematochezia without abdominal pain
History of diverticulosis
Colonic neoplasia Change in bowel habits
Chronic bleeding
Personal or family history of colon neoplasia
Weight loss
Ischemic colitis Cardiovascular disease
Hematochezia with or without abdominal pain
UC Bloody diarrhea
Family history of IBD
History of UC
Crohn disease Chronic abdominal discomfort
Family history of IBD
History of Crohn disease
Anal fissure Hematochezia with anal pain
Severe constipation
Hemorrhoids Dripping blood with bowel movements
Hematochezia with otherwise normal bowel movements
Postpolypectomy ulcer Recent colonoscopy with polypectomy
Use of anticoagulants or antiplatelet drugs
Colonic or small intestinal angioectasias Age >70 yr
Cardiovascular disease
Chronic LGI bleeding/iron deficiency anemia
Recurrent bleeding of variable severity
Anastomotic ulceration Prior intestinal surgical anastomosis
Radiation enteritis or proctitis History of abdominal radiation therapy
emesis or fresh bloody emesis that is witnessed do not require coagulation studies and for typing and crossmatching for packed
placement of an NG tube for diagnostic purposes but may need RBCs. The hematocrit or hemoglobin values immediately after
an NG tube to help clear the gastric blood for better endoscopic the onset of bleeding may not reflect blood loss accurately,
visualization and to minimize the risk of aspiration. because it takes more than 24 to 72 hours for the vascular space
to equilibrate with extravascular fluid and hemodilution results
5
Laboratory Studies from IV administration of saline. A mean corpuscular volume
(MCV) lower than 80 fL suggests chronic GI blood loss and iron
Blood from the patient with acute GI bleeding should be sent deficiency, which can be confirmed by the finding of low blood
for standard hematology, chemistry, liver biochemical, and iron, high total iron-binding capacity (TIBC), and low ferritin