Page 6 - Gastrointestinal Bleeding (Xuất huyết tiêu hóa)
P. 6
280 PART III Symptoms, Signs, and Biopsychosocial Issues
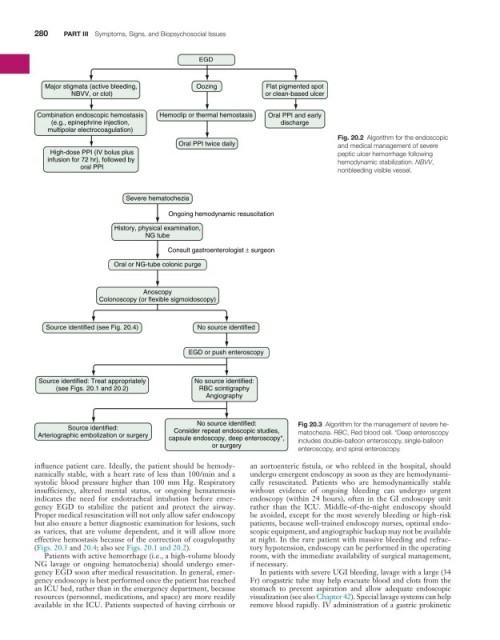
EGD
Major stigmata (active bleeding, Oozing Flat pigmented spot
NBVV, or clot) or clean-based ulcer
Combination endoscopic hemostasis Hemoclip or thermal hemostasis Oral PPI and early
(e.g., epinephrine injection, discharge
multipolar electrocoagulation)
Fig. 20.2 Algorithm for the endoscopic
Oral PPI twice daily and medical management of severe
High-dose PPI (IV bolus plus peptic ulcer hemorrhage following
infusion for 72 hr), followed by hemodynamic stabilization. NBVV,
oral PPI nonbleeding visible vessel.
Severe hematochezia
Ongoing hemodynamic resuscitation
History, physical examination,
NG tube
Consult gastroenterologist ± surgeon
Oral or NG-tube colonic purge
Anoscopy
Colonoscopy (or flexible sigmoidoscopy)
Source identified (see Fig. 20.4) No source identified
EGD or push enteroscopy
Source identified: Treat appropriately No source identified:
(see Figs. 20.1 and 20.2) RBC scintigraphy
Angiography
No source identified: Fig 20.3 Algorithm for the management of severe he-
Source identified: Consider repeat endoscopic studies,
Arteriographic embolization or surgery capsule endoscopy, deep enteroscopy*, matochezia. RBC, Red blood cell. *Deep enteroscopy
includes double-balloon enteroscopy, single-balloon
or surgery enteroscopy, and spiral enteroscopy.
influence patient care. Ideally, the patient should be hemody- an aortoenteric fistula, or who rebleed in the hospital, should
namically stable, with a heart rate of less than 100/min and a undergo emergent endoscopy as soon as they are hemodynami-
systolic blood pressure higher than 100 mm Hg. Respiratory cally resuscitated. Patients who are hemodynamically stable
insufficiency, altered mental status, or ongoing hematemesis without evidence of ongoing bleeding can undergo urgent
indicates the need for endotracheal intubation before emer- endoscopy (within 24 hours), often in the GI endoscopy unit
gency EGD to stabilize the patient and protect the airway. rather than the ICU. Middle-of-the-night endoscopy should
Proper medical resuscitation will not only allow safer endoscopy be avoided, except for the most severely bleeding or high-risk
but also ensure a better diagnostic examination for lesions, such patients, because well-trained endoscopy nurses, optimal endo-
as varices, that are volume dependent, and it will allow more scopic equipment, and angiographic backup may not be available
effective hemostasis because of the correction of coagulopathy at night. In the rare patient with massive bleeding and refrac-
(Figs. 20.3 and 20.4; also see Figs. 20.1 and 20.2). tory hypotension, endoscopy can be performed in the operating
Patients with active hemorrhage (i.e., a high-volume bloody room, with the immediate availability of surgical management,
NG lavage or ongoing hematochezia) should undergo emer- if necessary.
gency EGD soon after medical resuscitation. In general, emer- In patients with severe UGI bleeding, lavage with a large (34
gency endoscopy is best performed once the patient has reached Fr) orogastric tube may help evacuate blood and clots from the
an ICU bed, rather than in the emergency department, because stomach to prevent aspiration and allow adequate endoscopic
resources (personnel, medications, and space) are more readily visualization (see also Chapter 42). Special lavage systems can help
available in the ICU. Patients suspected of having cirrhosis or remove blood rapidly. IV administration of a gastric prokinetic