Page 7 - Gastrointestinal Bleeding (Xuất huyết tiêu hóa)
P. 7
CHAPTER 20 Gastrointestinal Bleeding 281
Severe hematochezia 20
Ongoing hemodynamic resuscitation
History, physical examination,
NG tube
History of cirrhosis, ulcers,
melena, or hematemesis History of hemorrhoids, No identifiable risk factors,
pelvic or abdominal painless hematochezia
radiation, colitis, diarrhea
EGD and/or
push enteroscopy
Anoscopy and flexible sigmoidoscopy
Source No source Source identified: No source identified
identified: identifed Treat
Treat
Colonic purge and urgent
colonoscopy
No source identified:
Push enteroscopy Source identified: Treat
Source identified: No source identified:
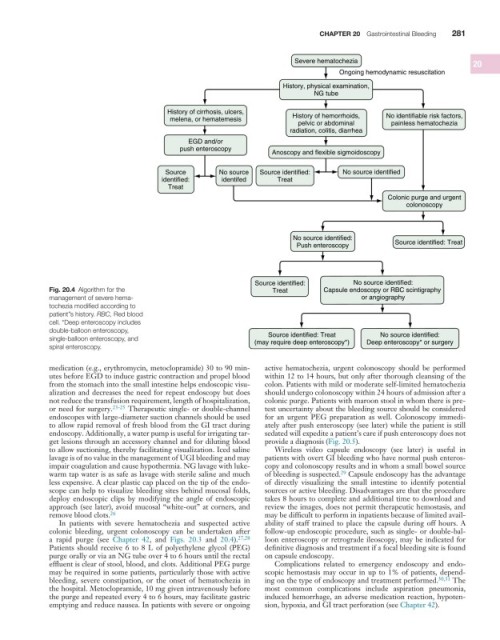
Fig. 20.4 Algorithm for the Treat Capsule endoscopy or RBC scintigraphy
management of severe hema- or angiography
tochezia modified according to
patient’’s history. RBC, Red blood
cell. *Deep enteroscopy includes
double-balloon enteroscopy,
No source identified:
Source identified: Treat
single-balloon enteroscopy, and (may require deep enteroscopy*) Deep enteroscopy* or surgery
spiral enteroscopy.
medication (e.g., erythromycin, metoclopramide) 30 to 90 min- active hematochezia, urgent colonoscopy should be performed
utes before EGD to induce gastric contraction and propel blood within 12 to 14 hours, but only after thorough cleansing of the
from the stomach into the small intestine helps endoscopic visu- colon. Patients with mild or moderate self-limited hematochezia
alization and decreases the need for repeat endoscopy but does should undergo colonoscopy within 24 hours of admission after a
not reduce the transfusion requirement, length of hospitalization, colonic purge. Patients with maroon stool in whom there is pre-
or need for surgery. 23-25 Therapeutic single- or double-channel test uncertainty about the bleeding source should be considered
endoscopes with large-diameter suction channels should be used for an urgent PEG preparation as well. Colonoscopy immedi-
to allow rapid removal of fresh blood from the GI tract during ately after push enteroscopy (see later) while the patient is still
endoscopy. Additionally, a water pump is useful for irrigating tar- sedated will expedite a patient’s care if push enteroscopy does not
get lesions through an accessory channel and for diluting blood provide a diagnosis (Fig. 20.5).
to allow suctioning, thereby facilitating visualization. Iced saline Wireless video capsule endoscopy (see later) is useful in
lavage is of no value in the management of UGI bleeding and may patients with overt GI bleeding who have normal push enteros-
impair coagulation and cause hypothermia. NG lavage with luke- copy and colonoscopy results and in whom a small bowel source
warm tap water is as safe as lavage with sterile saline and much of bleeding is suspected. Capsule endoscopy has the advantage
29
less expensive. A clear plastic cap placed on the tip of the endo- of directly visualizing the small intestine to identify potential
scope can help to visualize bleeding sites behind mucosal folds, sources or active bleeding. Disadvantages are that the procedure
deploy endoscopic clips by modifying the angle of endoscopic takes 8 hours to complete and additional time to download and
approach (see later), avoid mucosal “white-out” at corners, and review the images, does not permit therapeutic hemostasis, and
remove blood clots. 26 may be difficult to perform in inpatients because of limited avail-
In patients with severe hematochezia and suspected active ability of staff trained to place the capsule during off hours. A
colonic bleeding, urgent colonoscopy can be undertaken after follow-up endoscopic procedure, such as single- or double-bal-
a rapid purge (see Chapter 42, and Figs. 20.3 and 20.4). 27,28 loon enteroscopy or retrograde ileoscopy, may be indicated for
Patients should receive 6 to 8 L of polyethylene glycol (PEG) definitive diagnosis and treatment if a focal bleeding site is found
purge orally or via an NG tube over 4 to 6 hours until the rectal on capsule endoscopy.
effluent is clear of stool, blood, and clots. Additional PEG purge Complications related to emergency endoscopy and endo-
may be required in some patients, particularly those with active scopic hemostasis may occur in up to 1% of patients, depend-
bleeding, severe constipation, or the onset of hematochezia in ing on the type of endoscopy and treatment performed. 30,31 The
the hospital. Metoclopramide, 10 mg given intravenously before most common complications include aspiration pneumonia,
the purge and repeated every 4 to 6 hours, may facilitate gastric induced hemorrhage, an adverse medication reaction, hypoten-
emptying and reduce nausea. In patients with severe or ongoing sion, hypoxia, and GI tract perforation (see Chapter 42).