Page 11 - RTF.20 Employee Benefits
P. 11
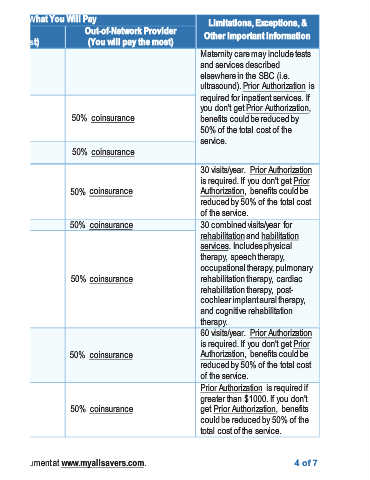
Exceptions, & Other Important Information ultrasound). Prior Authorization is visits/year. Prior Authorization occupational therapy, pulmonary Prior Authorization is required if benefits 4of 7
Limitations, Maternity care may include tests and services described elsewhere in the SBC (i.e. required for inpatient services. If you don't get Prior Authorization, benefits could be reduced by 50% of the total cost of the service. 30 is required. If you don't get Prior Authorization, benefits could be reduced by 50% of the total cost of the service. 30 combined visits/year for rehabilitation and habilitation services. Includes physical therapy, sp
Out-of-Network Provider (You will pay the most) coinsurance coinsurance coinsurance coinsurance coinsurance coinsurance coinsurance
What You Will Pay 50% 50% 50% 50% 50% 50% 50%
Network Provider (You will pay the least) Deductible does not apply. coinsurance coinsurance coinsurance coinsurance coinsurance coinsurance coinsurance * For more information about limitations and exceptions, see the plan or policy document at www.myallsavers.com.
Services You May Need Childbirth/delivery 0% professional services Childbirth/delivery 0% facility services 0% Home health care 0% Rehabilitation services 0% Habilitation services 0% Skilled nursing care Durable medical 0% equipment
Common Medical Event If you need help recovering or have other special health needs