Page 9 - RTF.20 Employee Benefits
P. 9
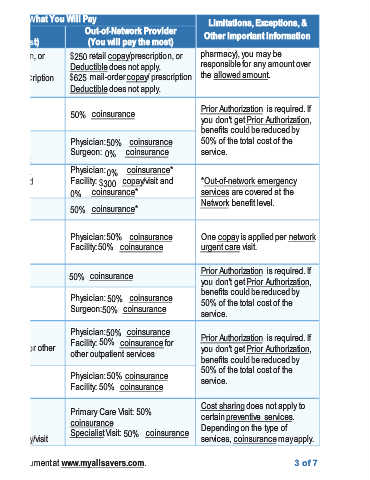
Exceptions, & Other Important Information is required. If One copay is applied per network is required. If is required. If services. services, coinsurance may apply. 3of 7
Limitations, pharmacy), you may be responsible for any amount over the allowed amount. Prior Authorization you don't get Prior Authorization, benefits could be reduced by 50% of the total cost of the service. *Out-of-network emergency services are covered at the Network benefit level. urgent care visit. Prior Authorization you don't get Prior Authorization, benefits could be reduced by 50% of the total cost of the service. Prior Authorization y
Out-of-Network Provider (You will pay the most) retail copay/prescription, or Deductible does not apply. mail-order copay/ prescription Deductible does not apply. coinsurance Physician: coinsurance 50% Surgeon: coinsurance 0% Physician: coinsurance* 0% Facility: copay/visit and $300 coinsurance* coinsurance* 50% Physician: coinsurance Facility:
What You Will Pay $250 $625 50% 0% 50% 50% coinsurance
Network Provider (You will pay the least) retail copay/prescription, or $250 Deductible does not apply. mail-order copay/ prescription $625 Deductible does not apply. coinsurance Physician: copay/visit $60 Deductible does not apply. Surgeon: coinsurance 0% 0% Physician: coinsurance Facility: copay/visit and $300 $30 coinsurance 0% coinsurance Physician:
Services You May Need Tier 4 drugs Facility fee (e.g., 0% ambulatory surgery center) Physician/surgeon fees Emergency room services Emergency medical 0% transportation Urgent care Facility fee (e.g., 0% hospital room) Physician/surgeon fees Outpatient services Inpatient services Office visits
Common Medical Event If you have outpatient surgery If you need immediate medical attention If you have a hospital stay If you need mental health, behavioral health, or substance abuse services If you are pregnant