Page 63 - Fluid, Electrolyte, and Acid-Base Disorders in Small Animal Practice
P. 63
Disorders of Sodium and Water: Hypernatremia and Hyponatremia 53
Collecting duct Tubular
Blood Interstitial fluid principal cell fluid
NSAIDs Demeclocycline
– Halothane
Lithium
Renal prostaglandins (PGE2, PGI2) Methoxyflurane
+ – –
AQP3 AQP2
vesicle
H 2O
5' AMP
Alpha adrenergic drugs
E. coli endotoxin PDE Inactive
Glucocorticoids – PKA
Hypercalcemia cAMP H 2O
Hypokalemia Active
AC
PKA AQP2
H 2O
ATP
Antidiuretic V2 G s-GTP H 2O
P
hormone
H 2O
(vasopressin) G s-GDP P P
Chlorpropamide +
Basolateral
membrane
P luminal
H 2O
Phosphorylated membrane
AQP4 AQP2 vesicle
Barbiturates Narcotics
+ Beta adrenergic drugs Nicotine
Carbamazepine Nitrous oxide
Ethanol – Cholinergic drugs Tricyclic antidepressants
Glucocorticoids Chlorpropamide Vincristine
Phenytoin Clofibrate
+ Plasma hyperosmolality Nausea
Pain
Volume depletion Anxiety
Neurohypophysis
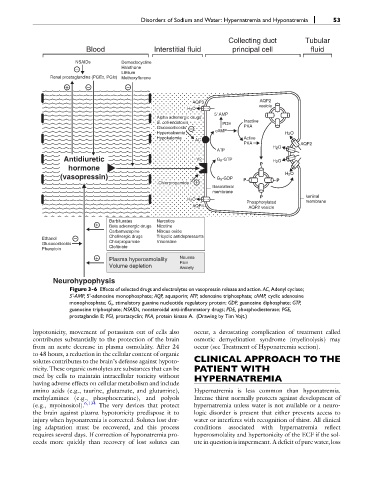
Figure 3-6 Effects of selected drugs and electrolytes on vasopressin release and action. AC, Adenyl cyclase;
5'-AMP, 5'-adenosine monophosphate; AQP, aquaporin; ATP, adenosine triphosphate; cAMP, cyclic adenosine
monophosphate; G s , stimulatory guanine nucleotide regulatory protein; GDP, guanosine diphosphate; GTP,
guanosine triphosphate; NSAIDs, nonsteroidal anti-inflammatory drugs; PDE, phosphodiesterase; PGE,
prostaglandin E; PGI, prostacyclin; PKA, protein kinase A. (Drawing by Tim Vojt.)
hypotonicity, movement of potassium out of cells also occur, a devastating complication of treatment called
contributes substantially to the protection of the brain osmotic demyelination syndrome (myelinolysis) may
from an acute decrease in plasma osmolality. After 24 occur (see Treatment of Hyponatremia section).
to 48 hours, a reduction in the cellular content of organic
solutes contributes to the brain’s defense against hypoto- CLINICAL APPROACH TO THE
nicity. These organic osmolytes are substances that can be PATIENT WITH
used by cells to maintain intracellular tonicity without HYPERNATREMIA
having adverse effects on cellular metabolism and include
amino acids (e.g., taurine, glutamate, and glutamine), Hypernatremia is less common than hyponatremia.
methylamines (e.g., phosphocreatine), and polyols Intense thirst normally protects against development of
(e.g., myoinositol). 6,134 The very devices that protect hypernatremia unless water is not available or a neuro-
the brain against plasma hypotonicity predispose it to logic disorder is present that either prevents access to
injury when hyponatremia is corrected. Solutes lost dur- water or interferes with recognition of thirst. All clinical
ing adaptation must be recovered, and this process conditions associated with hypernatremia reflect
requires several days. If correction of hyponatremia pro- hyperosmolality and hypertonicity of the ECF if the sol-
ceeds more quickly than recovery of lost solutes can ute in question is impermeant. A deficit of pure water, loss