Page 495 - Withrow and MacEwen's Small Animal Clinical Oncology, 6th Edition
P. 495
CHAPTER 23 Cancer of the Gastrointestinal Tract 473
VetBooks.ir
A
A
Metastatic Medial lliac Lymph Node
Internal lliac Artery
Internal lliac Vein
B B
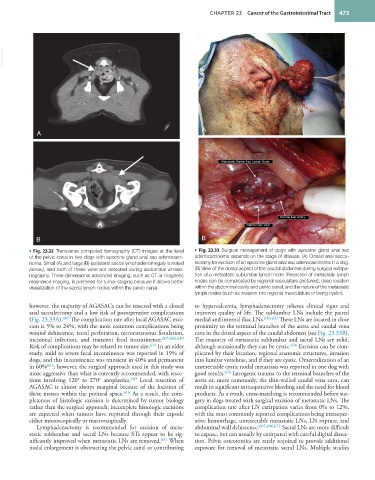
• Fig. 23.32 Transverse computed tomography (CT) images at the level • Fig. 23.33 Surgical management of dogs with apocrine gland anal sac
of the pelvic canal in two dogs with apocrine gland anal sac adenocarci- adenocarcinoma depends on the stage of disease. (A) Closed anal saccu-
noma. Small (A) and large (B) ipsilateral sacral lymphadenomegaly is noted lectomy for excision of an apocrine gland anal sac adenocarcinoma in a dog.
(arrow), and both of these were not detected during abdominal ultraso- (B) View of the dorsal aspect of the caudal abdomen during surgical extirpa-
nography. Three-dimensional advanced imaging, such as CT or magnetic tion of a metastatic sublumbar lymph node. Resection of metastatic lymph
resonance imaging, is preferred for tumor staging because it allows better nodes can be complicated by regional vasculature (pictured), deep location
visualization of the sacral lymph nodes within the pelvic canal. within the abdominal cavity and pelvic canal, and the nature of the metastatic
lymph nodes (such as invasion into regional musculature or being cystic).
however, the majority of AGASACs can be resected with a closed to hypercalcemia, lymphadenectomy relieves clinical signs and
anal sacculectomy and a low risk of postoperative complications improves quality of life. The sublumbar LNs include the paired
(Fig. 23.33A). 605 The complication rate after local AGASAC exci- medial and internal iliac LNs. 630,631 These LNs are located in close
sion is 5% to 24%, with the most common complications being proximity to the terminal branches of the aorta and caudal vena
wound dehiscence, rectal perforation, rectocutaneous fistulation, cava in the dorsal aspect of the caudal abdomen (see Fig. 23.33B).
incisional infection, and transient fecal incontinence. 605,606,610 The majority of metastatic sublumbar and sacral LNs are solid,
Risk of complications may be related to tumor size. 610 In an older although occasionally they can be cystic. 636 Excision can be com-
study, mild to severe fecal incontinence was reported in 19% of plicated by their location, regional anatomic structures, invasion
dogs, and this incontinence was transient in 40% and permanent into lumbar vertebrae, and if they are cystic. Omentalization of an
in 60% 603 ; however, the surgical approach used in this study was unresectable cystic nodal metastasis was reported in one dog with
more aggressive than what is currently recommended, with resec- good results. 636 Iatrogenic trauma to the terminal branches of the
tions involving 120° to 270° anoplasties. 603 Local resection of aorta or, more commonly, the thin-walled caudal vena cava, can
AGASAC is almost always marginal because of the location of result in significant intraoperative bleeding and the need for blood
these masses within the perineal space. 616 As a result, the com- products. As a result, cross-matching is recommended before sur-
pleteness of histologic excision is determined by tumor biology gery in dogs treated with surgical excision of metastatic LNs. The
rather than the surgical approach; incomplete histologic excisions complication rate after LN extirpation varies from 0% to 12%,
are expected when tumors have ruptured through their capsule with the most commonly reported complications being intraoper-
either microscopically or macroscopically. ative hemorrhage, unresectable metastatic LNs, LN rupture, and
Lymphadenectomy is recommended for excision of meta- abdominal wall dehiscence. 605,606,612 Sacral LNs are more difficult
static sublumbar and sacral LNs because STs appear to be sig- to expose, but can usually by extirpated with careful digital dissec-
nificantly improved when metastatic LNs are removed. 601 When tion. Pelvic osteotomies are rarely required to provide additional
nodal enlargement is obstructing the pelvic canal or contributing exposure for removal of metastatic sacral LNs. Multiple studies