Page 89 - Withrow and MacEwen's Small Animal Clinical Oncology, 6th Edition
P. 89
68 PART I The Biology and Pathogenesis of Cancer
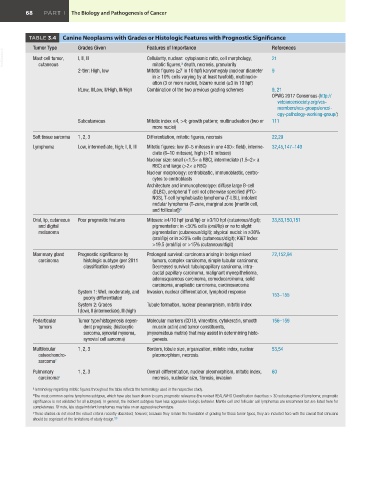
TABLE 3.4 Canine Neoplasms with Grades or Histologic Features with Prognostic Significance
Tumor Type Grades Given Features of Importance References
VetBooks.ir Mast cell tumor, I, II, III Cellularity, nuclear: cytoplasmic ratio, cell morphology, 21
cutaneous
mitotic figures, depth, necrosis, granularity
a
2-tier: High, low Mitotic figures (≥7 in 10 hpf) karyomegaly (nuclear diameter 9
in ≥ 10% cells varying by at least twofold), multinucle-
ation (3 or more nuclei), bizarre nuclei (≥3 in 10 hpf)
I/Low, II/Low, II/High, III/High Combination of the two previous grading schemes 9, 21
OPWG 2017 Consensus (http://
vetcancersociety.org/vcs-
members/vcs-groups/oncol-
ogy-pathology-working-group/)
Subcutaneous Mitotic index ≤4, >4; growth pattern; multinucleation (two or 111
more nuclei)
Soft tissue sarcoma 1, 2, 3 Differentiation, mitotic figures, necrosis 22,29
Lymphoma Low, intermediate, high; I, II, III Mitotic figures: low (0–5 mitoses in one 400× field), interme- 32,45,147–149
diate (6–10 mitoses), high (>10 mitoses)
Nuclear size: small (<1.5× a RBC), intermediate (1.5–2× a
RBC) and large (>2× a RBC)
Nuclear morphology: centroblastic, immunoblastic, centro-
cytes to centroblasts
Architecture and immunophenotype: diffuse large B-cell
(DLBC), peripheral T cell not otherwise specified (PTC-
NOS), T-cell lymphoblastic lymphoma (T-LBL), indolent
nodular lymphoma (T-zone, marginal zone [mantle cell,
and follicular]) b
Oral, lip, cutaneous Poor prognostic features Mitoses: ≥4/10 hpf (oral/lip) or ≥3/10 hpf (cutaneous/digit); 33,83,150,151
and digital pigmentation: in <50% cells (oral/lip) or no to slight
melanoma pigmentation (cutaneous/digit); atypical nuclei: in ≥30%
(oral/lip) or in ≥20% cells (cutaneous/digit); Ki67 Index:
>19.5 (oral/lip) or >15% (cutaneous/digit)
Mammary gland Prognostic significance by Prolonged survival: carcinoma arising in benign mixed 72,152,94
carcinoma histologic subtype (per 2011 tumors, complex carcinoma, simple tubular carcinoma;
classification system) Decreased survival: tubulopapillary carcinoma, intra-
ductal papillary carcinoma, malignant myoepithelioma,
adenosquamous carcinoma, comedocarcinoma, solid
carcinoma, anaplastic carcinoma, carcinosarcoma
System 1: Well, moderately, and Invasion, nuclear differentiation, lymphoid response 153–155
poorly differentiated
System 2: Grades Tubule formation, nuclear pleomorphism, mitotic index
I (low), II (intermediate), III (high)
Periarticular Tumor type/histogenesis depen- Molecular markers (CD18, vimentins, cytokeratin, smooth 156–159
tumors dent prognosis; (histiocytic muscle actin) and tumor constituents,
sarcoma, synovial myxoma, (myxomatous matrix) that may assist in determining histo-
synovial cell sarcoma) genesis.
Multilobular 1, 2, 3 Borders, lobule size, organization, mitotic index, nuclear 53,54
osteochondro- pleomorphism, necrosis
sarcoma c
Pulmonary 1, 2, 3 Overall differentiation, nuclear pleomorphism, mitotic index, 60
carcinoma c necrosis, nucleolar size, fibrosis, invasion
a Terminology regarding mitotic figures throughout the table reflects the terminology used in the respective study.
b The most common canine lymphoma subtypes, which have also been shown to carry prognostic relevance (the revised REAL/WHO Classification describes > 30 subcategories of lymphoma; prognostic
significance is not validated for all subtypes). In general, the indolent subtypes have less aggressive biologic behavior. Mantle cell and follicular cell lymphomas are uncommon but are listed here for
completeness. Of note, late stage indolent lymphomas may take on an aggressive phenotype.
c These studies do not meet the robust criteria recently described; however, because they remain the foundation of grading for these tumor types, they are included here with the caveat that clinicians
should be cognizant of the limitations of study design. 50