Page 35 - 2021 Medical Plan SPD
P. 35
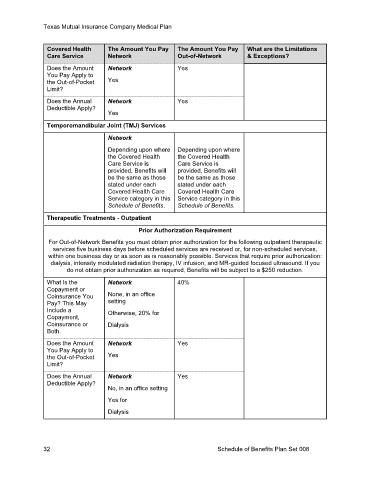
Texas Mutual Insurance Company Medical Plan
Covered Health The Amount You Pay The Amount You Pay What are the Limitations
Care Service Network Out-of-Network & Exceptions?
Does the Amount Network Yes
You Pay Apply to
the Out-of-Pocket Yes
Limit?
Does the Annual Network Yes
Deductible Apply?
Yes
Temporomandibular Joint (TMJ) Services
Network
Depending upon where Depending upon where
the Covered Health the Covered Health
Care Service is Care Service is
provided, Benefits will provided, Benefits will
be the same as those be the same as those
stated under each stated under each
Covered Health Care Covered Health Care
Service category in this Service category in this
Schedule of Benefits. Schedule of Benefits.
Therapeutic Treatments - Outpatient
Prior Authorization Requirement
For Out-of-Network Benefits you must obtain prior authorization for the following outpatient therapeutic
services five business days before scheduled services are received or, for non-scheduled services,
within one business day or as soon as is reasonably possible. Services that require prior authorization:
dialysis, intensity modulated radiation therapy, IV infusion, and MR-guided focused ultrasound. If you
do not obtain prior authorization as required, Benefits will be subject to a $250 reduction.
What Is the Network 40%
Copayment or
Coinsurance You None, in an office
Pay? This May setting
Include a Otherwise, 20% for
Copayment,
Coinsurance or Dialysis
Both.
Does the Amount Network Yes
You Pay Apply to
the Out-of-Pocket Yes
Limit?
Does the Annual Network Yes
Deductible Apply?
No, in an office setting
Yes for
Dialysis
32 Schedule of Benefits Plan Set 008