Page 32 - 2021 Medical Plan SPD
P. 32
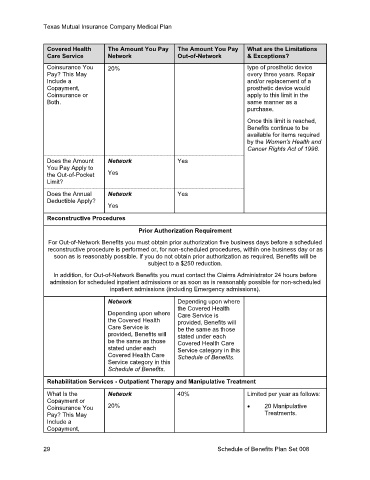
Texas Mutual Insurance Company Medical Plan
Covered Health The Amount You Pay The Amount You Pay What are the Limitations
Care Service Network Out-of-Network & Exceptions?
Coinsurance You 20% type of prosthetic device
Pay? This May every three years. Repair
Include a and/or replacement of a
Copayment, prosthetic device would
Coinsurance or apply to this limit in the
Both. same manner as a
purchase.
Once this limit is reached,
Benefits continue to be
available for items required
by the Women's Health and
Cancer Rights Act of 1998.
Does the Amount Network Yes
You Pay Apply to
the Out-of-Pocket Yes
Limit?
Does the Annual Network Yes
Deductible Apply?
Yes
Reconstructive Procedures
Prior Authorization Requirement
For Out-of-Network Benefits you must obtain prior authorization five business days before a scheduled
reconstructive procedure is performed or, for non-scheduled procedures, within one business day or as
soon as is reasonably possible. If you do not obtain prior authorization as required, Benefits will be
subject to a $250 reduction.
In addition, for Out-of-Network Benefits you must contact the Claims Administrator 24 hours before
admission for scheduled inpatient admissions or as soon as is reasonably possible for non-scheduled
inpatient admissions (including Emergency admissions).
Network Depending upon where
the Covered Health
Depending upon where Care Service is
the Covered Health provided, Benefits will
Care Service is be the same as those
provided, Benefits will stated under each
be the same as those Covered Health Care
stated under each Service category in this
Covered Health Care Schedule of Benefits.
Service category in this
Schedule of Benefits.
Rehabilitation Services - Outpatient Therapy and Manipulative Treatment
What Is the Network 40% Limited per year as follows:
Copayment or
Coinsurance You 20% • 20 Manipulative
Pay? This May Treatments.
Include a
Copayment,
29 Schedule of Benefits Plan Set 008