Page 33 - 2021 Medical Plan SPD
P. 33
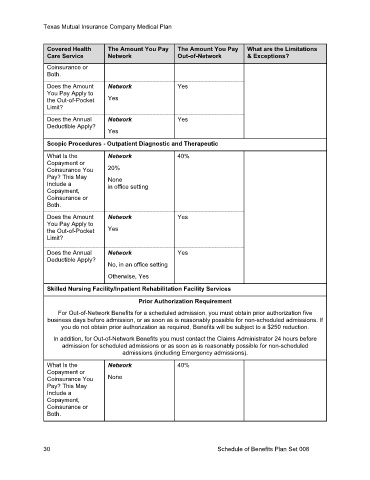
Texas Mutual Insurance Company Medical Plan
Covered Health The Amount You Pay The Amount You Pay What are the Limitations
Care Service Network Out-of-Network & Exceptions?
Coinsurance or
Both.
Does the Amount Network Yes
You Pay Apply to
the Out-of-Pocket Yes
Limit?
Does the Annual Network Yes
Deductible Apply?
Yes
Scopic Procedures - Outpatient Diagnostic and Therapeutic
What Is the Network 40%
Copayment or
Coinsurance You 20%
Pay? This May None
Include a in office setting
Copayment,
Coinsurance or
Both.
Does the Amount Network Yes
You Pay Apply to
the Out-of-Pocket Yes
Limit?
Does the Annual Network Yes
Deductible Apply?
No, in an office setting
Otherwise, Yes
Skilled Nursing Facility/Inpatient Rehabilitation Facility Services
Prior Authorization Requirement
For Out-of-Network Benefits for a scheduled admission, you must obtain prior authorization five
business days before admission, or as soon as is reasonably possible for non-scheduled admissions. If
you do not obtain prior authorization as required, Benefits will be subject to a $250 reduction.
In addition, for Out-of-Network Benefits you must contact the Claims Administrator 24 hours before
admission for scheduled admissions or as soon as is reasonably possible for non-scheduled
admissions (including Emergency admissions).
What Is the Network 40%
Copayment or
Coinsurance You None
Pay? This May
Include a
Copayment,
Coinsurance or
Both.
30 Schedule of Benefits Plan Set 008