Page 9 - PetVet 2022 Master Benefits Guide_Final
P. 9
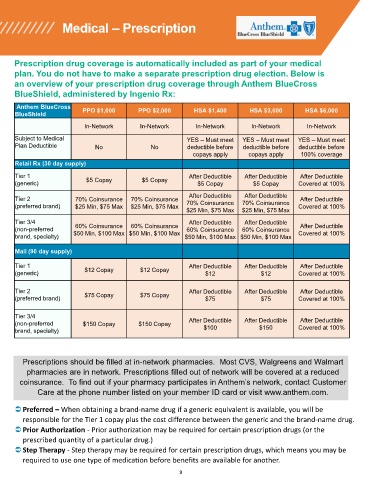
Medical – Prescription
Prescription drug coverage is automatically included as part of your medical
plan. You do not have to make a separate prescription drug election. Below is
an overview of your prescription drug coverage through Anthem BlueCross
BlueShield, administered by Ingenio Rx:
Anthem BlueCross
PPO $1,000 PPO $2,000 HSA $1,400 HSA $3,000 HSA $6,000
BlueShield
In-Network In-Network In-Network In-Network In-Network
Subject to Medical YES – Must meet YES – Must meet YES – Must meet
Plan Deductible No No deductible before deductible before deductible before
copays apply copays apply 100% coverage
Retail Rx (30 day supply)
Tier 1 After Deductible After Deductible After Deductible
$5 Copay $5 Copay
(generic) $5 Copay $5 Copay Covered at 100%
After Deductible After Deductible
Tier 2 70% Coinsurance 70% Coinsurance After Deductible
(preferred brand) $25 Min, $75 Max $25 Min, $75 Max 70% Coinsurance 70% Coinsurance Covered at 100%
$25 Min, $75 Max $25 Min, $75 Max
Tier 3/4 After Deductible After Deductible
(non-preferred 60% Coinsurance 60% Coinsurance 60% Coinsurance 60% Coinsurance After Deductible
brand, specialty) $50 Min, $100 Max $50 Min, $100 Max $50 Min, $100 Max $50 Min, $100 Max Covered at 100%
Mail (90 day supply)
Tier 1 After Deductible After Deductible After Deductible
$12 Copay $12 Copay
(generic) $12 $12 Covered at 100%
Tier 2 After Deductible After Deductible After Deductible
(preferred brand) $75 Copay $75 Copay $75 $75 Covered at 100%
Tier 3/4
After Deductible After Deductible After Deductible
(non-preferred $150 Copay $150 Copay
brand, specialty) $100 $150 Covered at 100%
Prescriptions should be filled at in-network pharmacies. Most CVS, Walgreens and Walmart
pharmacies are in network. Prescriptions filled out of network will be covered at a reduced
coinsurance. To find out if your pharmacy participates in Anthem’s network, contact Customer
Care at the phone number listed on your member ID card or visit www.anthem.com.
Preferred – When obtaining a brand-name drug if a generic equivalent is available, you will be
responsible for the Tier 1 copay plus the cost difference between the generic and the brand-name drug.
Prior Authorization - Prior authorization may be required for certain prescription drugs (or the
prescribed quantity of a particular drug.)
Step Therapy - Step therapy may be required for certain prescription drugs, which means you may be
required to use one type of medication before benefits are available for another.
9