Page 20 - 1800Flowers 2022 Benefits Guide
P. 20
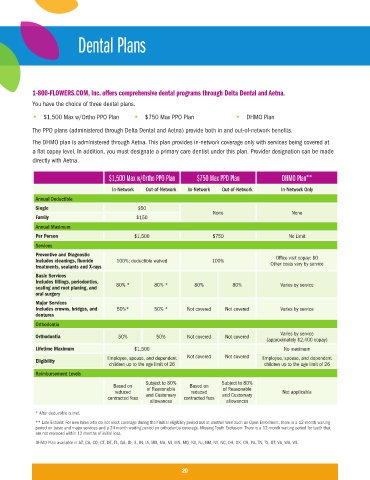
Dental Plans
1-800-FLOWERS.COM, Inc. offers comprehensive dental programs through Delta Dental and Aetna.
You have the choice of three dental plans.
• $1,500 Max w/Ortho PPO Plan • $750 Max PPO Plan • DHMO Plan
The PPO plans (administered through Delta Dental and Aetna) provide both in and out-of-network benefits.
The DHMO plan is administered through Aetna. This plan provides in-network coverage only with services being covered at
a flat copay level. In addition, you must designate a primary care dentist under this plan. Provider designation can be made
directly with Aetna.
$1,500 Max w/Ortho PPO Plan $750 Max PPO Plan DHMO Plan**
In-Network Out-of-Network In-Network Out-of-Network In-Network Only
Annual Deductible
Single $50
None None
Family $150
Annual Maximum
Per Person $1,500 $750 No Limit
Services
Preventive and Diagnostic Office visit copay: $0
Includes cleanings, fluoride 100%; deductible waived 100% Other costs vary by service
treatments, sealants and X-rays
Basic Services
Includes fillings, periodontics, 80% * 80% * 80% 80% Varies by service
scaling and root planing, and
oral surgery
Major Services
Includes crowns, bridges, and 50%* 50% * Not covered Not covered Varies by service
dentures
Orthodontia
Varies by service
Orthodontia 50% 50% Not covered Not covered
(approximately $2,400 copay)
Lifetime Maximum $1,500 No maximum
Eligibility Employee, spouse, and dependent Not covered Not covered Employee, spouse, and dependent
children up to the age limit of 26 children up to the age limit of 26
Reimbursement Levels
Subject to 80% Subject to 80%
Based on of Reasonable Based on of Reasonable
reduced reduced Not applicable
contracted fees and Customary contracted fees and Customary
allowances allowances
* After deductible is met.
** Late Entrant: For new hires who do not elect coverage during their initial eligibility period but at another time such as Open Enrollment, there is a 12-month waiting
period on basic and major services and a 24 month waiting period on orthodontia coverage. Missing Tooth Exclusion: There is a 12-month waiting period for teeth that
are not replaced within 12 months of initial loss.
DHMO Plan available in AZ, CA, CO, CT, DE, FL, GA, ID, IL, IN, IA, MD, MA, MI, MN, MO, NV, NJ, NM, NY, NC, OH, OK, OR, PA, TN, TX, UT, VA, WA, WI.
20