Page 10 - 2022 Insurity OE Guide FINAL
P. 10
UnitedHealthcare – Optum
Pharmacy Plan – Bin# 610279
As part of Insurity’s health plan, we have a pharmacy benefit manager through Optum. Although you use the same member
ID card for both medical and pharmacy, Optum is the company that manages our prescription medication costs for covered
members on our plans. Below is an outline of how our prescription drug plan works. We have three different prescription
tiers, based on the associated formularies:
O Tier 1 Rx – Lower-cost medications that provide the highest overall value. Mostly generic drugs. Some brand-name
drugs may also be included.
O Tier 2 Rx – Mid-range cost medications that provide good overall value. A mix of brand-name and generic drugs.
O Tier 3 Rx – Highest-cost medications that provide the lowest overall value. Mostly brand-name drugs, as well as
some generics.
Insurity uses Step Therapy as part of our pharmacy program. Step Therapy is a way to mitigate the high costs of prescription
medication when an effective, lower cost alternative is available.
If you have already tried lower cost alternatives or if there is a clinical reason for you to be taking the higher cost medication,
your provider can contact UHC/Optum to discuss available options.
You can check your medications and whether Step Therapy is required by clicking here:
www.uhcprovider.com/en/prior-auth-advance-notification/prior-auth-specialty-drugs/prior-auth-pharmacy-medical-
necessity.html
Please see the prescription drug list and approved list of preventive medications by logging into your portal: www.myuhc.com.
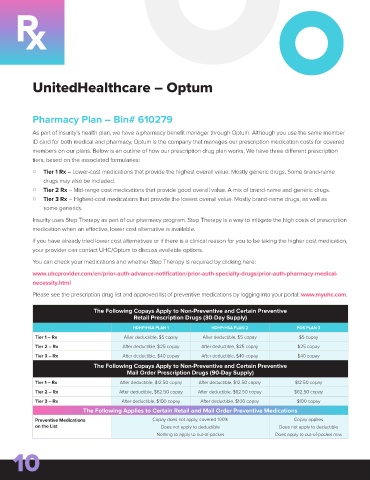
The Following Copays Apply to Non-Preventive and Certain Preventive
Retail Prescription Drugs (30-Day Supply)
HDHP/HSA PLAN 1 HDHP/HSA PLAN 2 POS PLAN 3
Tier 1 – Rx After deductible, $5 copay After deductible, $5 copay $5 copay
Tier 2 – Rx After deductible, $25 copay After deductible, $25 copay $25 copay
Tier 3 – Rx After deductible, $40 copay After deductible, $40 copay $40 copay
The Following Copays Apply to Non-Preventive and Certain Preventive
Mail Order Prescription Drugs (90-Day Supply)
Tier 1 – Rx After deductible, $12.50 copay After deductible, $12.50 copay $12.50 copay
Tier 2 – Rx After deductible, $62.50 copay After deductible, $62.50 copay $62.50 copay
Tier 3 – Rx After deductible, $100 copay After deductible, $100 copay $100 copay
The Following Applies to Certain Retail and Mail Order Preventive Medications
Preventive Medications Copay does not apply, covered 100% Copay applies
on the List Does not apply to deductible Does not apply to deductible
Nothing to apply to out-of-pocket Does apply to out-of-pocket max
10